Research Article Open Access
Peripheral Nerve Stimulation in Refractory Neuropathic Low Back Pain
Sylvie Raoul*, Emmanuelle Kuhn, Sylvain Durand, Jean-Paul N’Guyen and Julien Nizard
Service de Neurochirurgie, Centre Hospitalier Universitaire de Nantes, Nantes, France
- *Corresponding Author:
- Sylvie Raoul
Department of Neurosurgery, Centre Hospitalier Universitaire de Nantes
Bd jacques Monod, Nantes, 44000, France
Tel: 33621873262
Fax: 33240165301
E-mail: sylvie.raoul@chu-nantes.fr
Received date: June 20, 2016; Accepted date: July 18, 2016; Published date: July 21, 2016
Citation: Raoul S, Kuhn E, Durand S, N’Guyen JP, Nizard J (2013) Peripheral Nerve Stimulation in Refractory Neuropathic Low Back Pain. J Pain Relief S4:003. doi: 10.4172/2167-0846.S4-003
Copyright: © 2016 Raoul S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
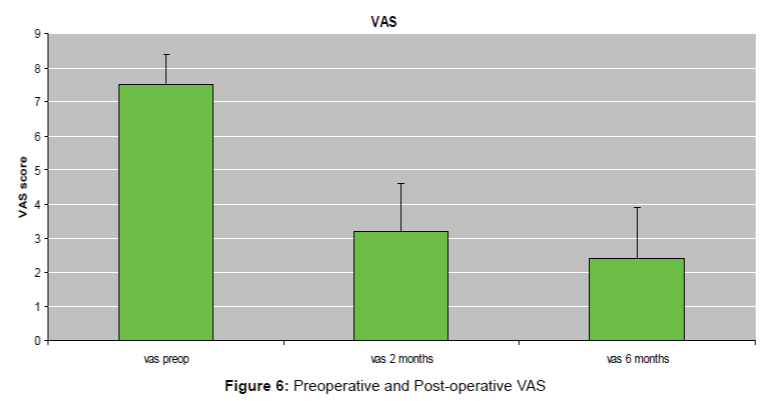
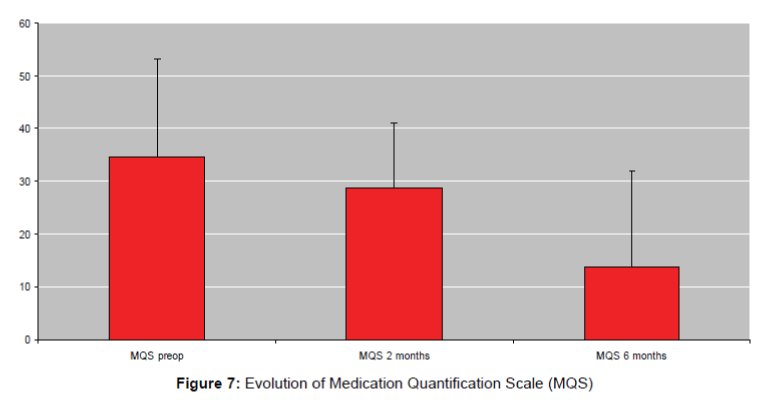
Introduction: Spinal cord stimulation is now a treatment of pain in refractory failed back surgery syndrome. The effect on radiculalgias is quite good but often unsatisfying to treat completely low back pain. Subcutaneous peripheral nerve stimulation is now one of the possibility to rescue chronic low back pain. The aim of this prospective study conducted in our center (Nantes, France) is to evaluate the benefit of the subcutaneous peripheral nerve stimulation on chronic low back pain. Method: 34 patients (aged 44-65, mean value 54.3) with chronic bilateral low back pain were evaluated with VAS Score, Medication quantification Scale (MQS), the patient satisfaction, and walking distance before and after stimulation. Stimulation was proposed after failure of multidisciplinary management of the patient with algologist, psychologist and rehabilitation. Electrode stimulation was implanted under local or general anesthesia and a test of 7 days was performed at home. The battery was implanted only if VAS score decreased than more 50%. Mean Follow up was 6 months (range 42 to 3 months). Result: All of 34 patients were implanted with good results: VAS score decreased from 7.5 in preoperative conditions to 2.3 in postop conditions (p ≤ 0.001). 63% of patients estimated than they were very satisfy of the surgery and they could propose that to patients. The MQS decreased from 34 in preoperative to 26 two months after the surgery and to 17 6 months after surgery. Walking distance increase after the surgery (800 meters before surgery and 1700 meters after surgery). We have 1 infection and one migration of electrodes Conclusion: this series shows that subcutaneous stimulation can be benefit to treat refractory low back pain. This surgery was well tolerated, safe.
Keywords
Peripheral nerve stimulation, Low back pain, Subcutaneous stimulation, Surgical treatment of low back pain
Introduction
Chronic low back pain affects approximately 25% of the general population and their direct and indirect costs are a major public health problem. Refractory chronic low back pains are defined by their rebellious character in a multidisciplinary management, including several treatment lines, including strong opioids, co-analgesics, functional and sometimes surgical management.
Chronic low back pain are typically of mixed origin: mechanical and neuropathic. According to N. Attal and ID. Beith, neuropathic component of low back pain varies between 8% and 16% for pure lumbago and between 80% and 96% for sciatica [1,2]. According Mimassi Thirty six percent of low back pain refractory supported in the assessment and treatment centers of the pain have a predominant neuropathic component [3].
It is in this context of chronic pain with a neuropathic component, the subcutaneous neurostimulation techniques have developed. Various indications were examined: occipital neuralgia, the face of pain, the abdomen, groin, pelvis and lumbar finally [4,5]. These neurostimulation techniques involve placing electrodes in adipose subcutaneous tissue at the base of the painful area and not in contact with the main nerve innervating the painful area. The evolution of the electrodes, the cross-priming (cross-talk) and the best electrical conduction into the fatty tissue (100 to 1000 times greater than that of the skin) have increased the surface of stimulated areas, covering several metameric levels [6].
While spinal cord stimulation has proven effective in support of the refractory chronic radicular pain, it remained insufficient for the treatment of chronic low back pain, especially due to difficulties in covering several metameres and thus a sufficiently large surface [7-9]. Several case studies have reported the efficacy of stimulation lumbar subcutaneous associated with a spinal cord stimulation for chronic lombosciatalgies [10-13]. Others have reported the efficacy of stimulation subcutaneous only in cases of chronic pain postsurgical axial Rebel [14-19].
Methodology
Anatomy and physiopathology
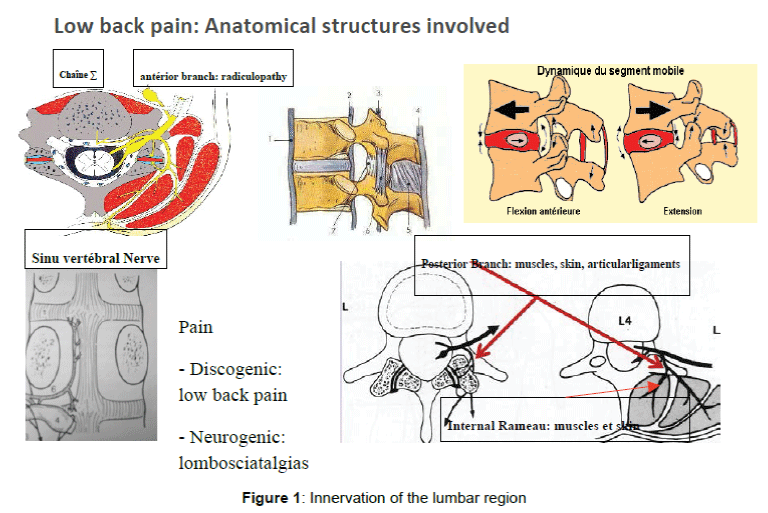
Several structures are involved in low back pain: intervertebral disc, facet joints, muscles and integument. The pain is often mixed with mechanical low back pain and neuropathic low back pain. The characteristics of these pains are quite different and their treatment will be adapted to the type of back pain. The intervertebral disc is innervated in part by the sympathetic chain through the sinu-vertebral nerve. There is a convergence of the sinu- vertebral nerve L5-S1 levels L4-L5, L3-L4 on the twig from L1-L2 [20]. Thus in pure discogenic low back pain infiltration sinu-vertebral nerve in L-L2 may allow resolution of these low back pain. The other innervation system is linked to the rear branch of the nerve root which supports the articular processes posterior muscles and testa Cf; (Figure 1) if this system is generally metameric there are wide anastomoses the metameres possibly responsible for referred pain. it is this system that is involved in sub lumbar cutaneous stimulation. Indeed as the gate-control theory of Wall Melzach and the stimulation of the large Aα fibers allows the activation of inhibitory collateral to reduce the intensity of pain mediated by small AD fibers and C. These fibers have a specific somatotopy at the spinal cord. They are often located in contact with the middle line, deep enough and the vertebral level Th9-Th10. this explains the difficulty encountered in encrocher these fibers by spinal cord stimulation.
Indications and contra-indications
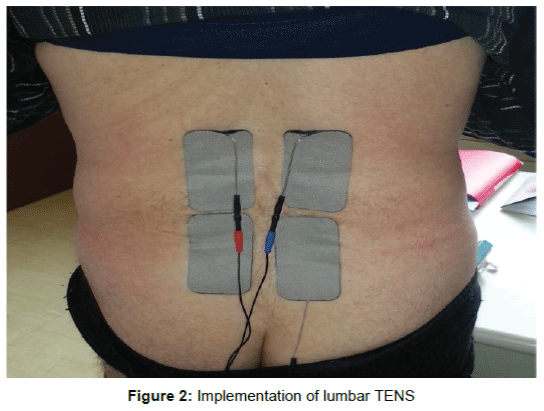
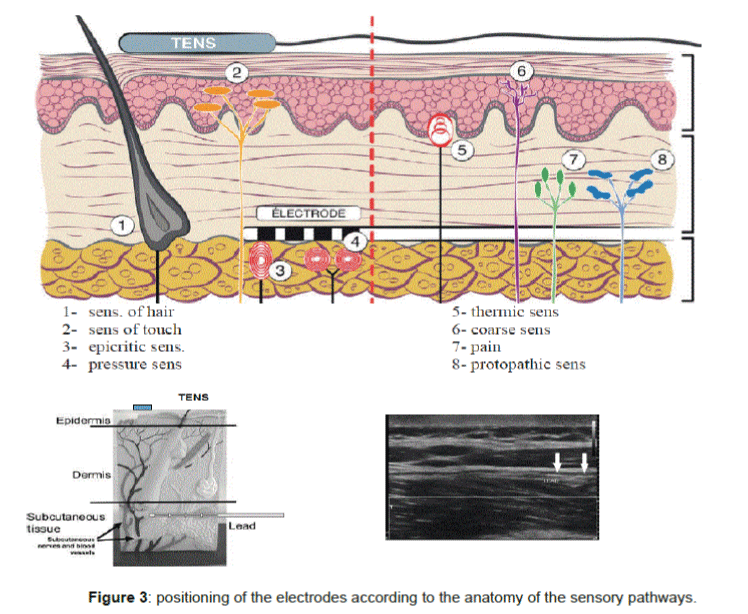
The sub cutaneous lumbar stimulation is indicated in chronic low back pain for more than 6 months, with neuropathic allodynia, burns, vice sensation bar with DN4 ≥ 6/10. The management of these low back pains that can be pure or associated with radicular first have a drug therapy (NSAIDs, analgesics bearing 1 to 3, antiepileptic and antidepressant) and re- education in center and support on a central pain with psychological counseling. When all of this optimized multidisciplinary approach is failing, then discusses the establishment of sub lumbar cutaneous stimulation electrodes. The surgical management of proposal should not be too late to be able to consider a resumption of daily life and professional activities. The location decision should be multidisciplinary consultation to avoid the pitfalls of too much psychological fragility. Consistent with the literature [1] pure low back pain account for 8 to 16%, low back pain associated with radiculopathy from 80 to 96%, the lomboradiculalgies post FBSS 50%. Neuropathic component of low back pain will be even more important as there is an association with a nerve root and the patient has been operated in the lumbar region (FBSS). Good indications are of low back pain fail back surgery syndrome (FBSS), chronic low back pain on settlement or non-surgical fracture found no spinal instability. Preimplantation testing is often performed preoperatively with transcutaneous electrical stimulation (TENS) (Figure 2). However, a prospective randomized study of 236 patients found no difference between the TENS treatment group and the placebo group [3]. The predictive value of TENS is negative to assess the effectiveness of the sub lumbar skin stimulation (Figure 3). The main indications are against a compressive disc herniation found MRI to CT, spinal stenosis compression, depression unstabilized, untreated psychiatric illness.
Surgical techniques
Surgical techniques vary both in the type of electrodes used in the positioning thereof. Generally used electrodes percutaneous four contacts. The electrodes may be placed vertically or horizontally. Considering that the action mechanism uses the gate-control, the electrodes must be placed in the subcutaneous tissue to reach the nerves of conscious epicritic and proprioception. They should not be too superficial because there is a risk of skin erosion. If they are positioned too deeply stimulation may be unpleasant causing muscle contractions.
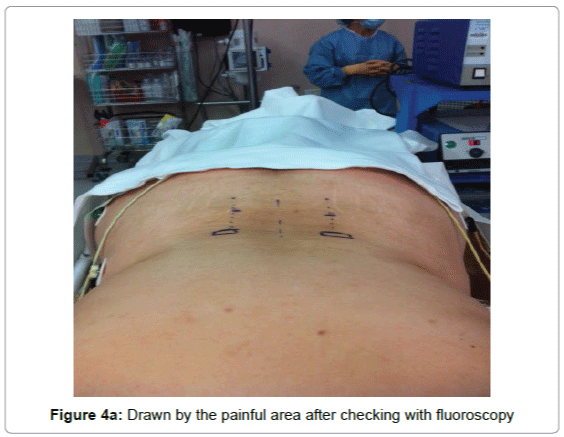
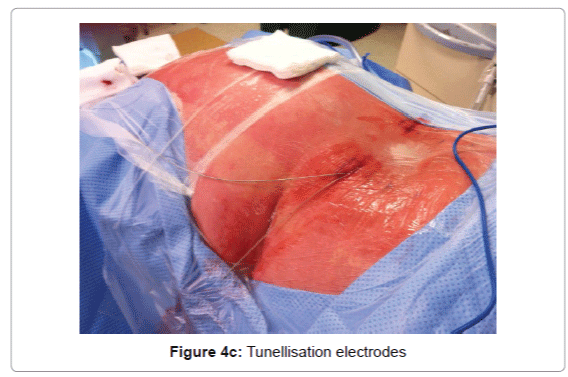
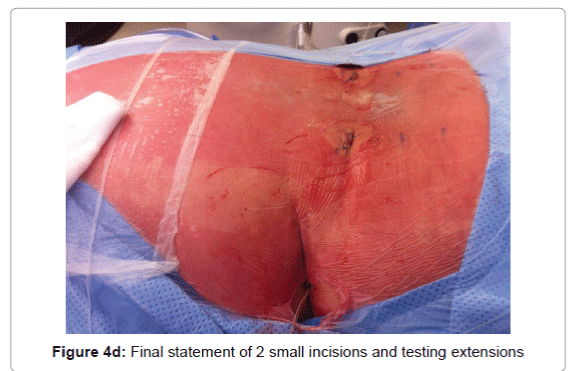
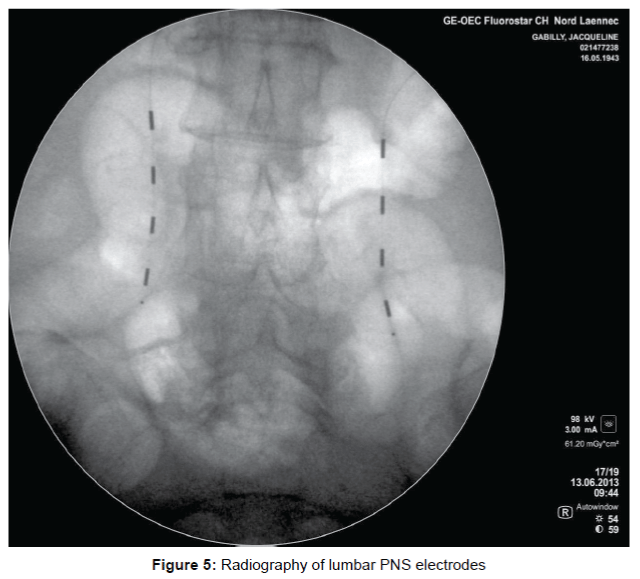
In our experience the implantation technique that allows the best coverage of the painful area with fewer side effects, is the implantation of percutaneous electrodes 2 4 studs longitudinally relative to the spine inserted by a Tuohy needle through 2 small incisions. The electrodes are then tunneled to the pacemaker implantation area (Figures 4a-5). The procedure is performed under local or general anesthesia. For the implantation of electrodes, a local or general anesthesia may be proposed. A test is performed at home for a week to 10 days and the pacemaker is then placed under general anesthesia for primary implantation or the electrodes are reconnected to the existing stimulator under general anesthesia.
Some authors have surgical electrodes [21] with a good result. In most of the series of subcutaneous stimulation literature is coupled to spinal cord stimulation. Indeed, spinal cord stimulation provides good coverage of radicular but covers less lumbar region [7,11]. With spinal cord electrode pads 4 or 8 and two broad percutaneous electrodes to four pads (Quad + Medtronic) it is possible to cross-stimulation that is more effective than the separate stimulation of two areas [7].
The three manufacturers (Medtronic, ANS and Boston) provide percutaneous electrodes for this type of stimulation. The choice of technology is left to the discretion of each surgeon.
Results of the Nantes Series and Review of Literature
We performed a retrospective study of 80 patients Assessment Centre and pain treatment Nantes University Hospital implanted stimulation subcutaneous lumbar between March 2011 and November 2015. These patients with low back pain chronic, lasting for more than 6 months, with or without radicular lower extremity, refractory to multiple treatment lines including strong opioids, co-analgesics, taking into functional and sometimes surgical management. All patients had subsequently received TENS with at least 50% improvement. The stimulator is started the day after surgery with the same parameters as those used during the test phase. The parameters are variable depending on the patient with 240 microsecond’s average (between 180 and 450 microseconds), a frequency of 50 Hz (40-70 HZ) and 3.2 V intensity (between 10.5 and 0.8 v). The settings are tuned to one month and 2 months post-op. 40 patients out of 80 suffering included radiculopathy lower limb associated with chronic low back pain. All were able to clearly differentiate these two pains. They already benefiting spinal cord stimulation for radicular pain, which did not cover the lumbar region, lumbar skin under electrodes have been added.
The long-term evaluation was conducted at 2 months and 6 months. The average duration of long-term follow-up was 11 months. 40 hommes and 40 women were implanted, average age 55 years, mean disease duration of 8.5 years of pain. The scales used were the EVA and the MQS. All patients had been evaluated on a pain center and were failing drug treatment, rehabilitation in failure and had psychological counseling. All the patients observed an improvement greater than 50% after the first surgical time, 80 patients were thus implanted subcutaneous neurostimulator. Statistical analysis by Wilcoxon test has shown that improved significantly (P ≤ 0.05). EVA goes from 7.5 to 2.4, the drug consumption is reduced by 39.5% (33.4 to 20.2 ± 1.2), the walking distance increases from 1600 meters to 2500 meters and there is a painful area reduction of 89%. (Figures 6 and 7).
All patients noted an improvement of all study endpoints. This significant improvement demonstrates the effectiveness of the treatment in addition, seems to represent a low surgical risk. Complications of the series are 4 infections (5%), epidural hematoma surgically taken without neurological deficit (1%) and two trips or electrode fracture (2.5%). Sator watched 13% of electrode displacement in 2009 [19]. Lumbar location, no mobile, coupled with a surgical attachment of electrodes to the subcutaneous plane probably explain this last point. Fourteen studies published in the literature (Table 1) in the lumbar skin stimulation. Six prospective series, nine retrospective series. Drastic reduction in pain scores. In the series of Mc Roberts EVA Password 7.8 preoperatively to 3.4 postoperation, in that of Yakovlev EVA Password 7.4 to 1.6 and that of Hamm-Faber EVA Password 6.2 3.2 . The overall improvement measured on the VAS of 72.8% (± 5.3) for all series.
| Author main recruiting year country | Study design | Number of patients implanted | Indications | Post-surgical pain |
|---|---|---|---|---|
| Burgher [19]USA monocetrique | Retrospective study | 6 | Neck pain,low back pain | 100% |
| Falco [7]USAmonocentrique | Prospective study | 18 | Headaches cervicogenic back pain back painpost- zoostérienne abdominal pain | 44% |
| Paicius[16]USAmono-centrique | Retrospective study | 6 | Low back pain | 83% |
| Sator[22]Autrichemulti-centrique | Retrospective study | 111 | Low back painlombosciatalgies neck pain post-herpetic | 56% |
| Verrils[18]Australiemono-centrique | Retrospective study | 14 | Low back pain | 85% |
| Verrils[15]Ausraliamono-centrique | 100 | Lumbosacralthoracic abdominal pelvic craniofacial | NR | |
| Yakovlev[17]USAmono-centrique | Retrospective study | 18 | Lombosciatalgies | 100% |
| Navarro [11]USA monocetrique | Retrospective study | 40 | Low back pain | 100% |
| Mironer[14]USA monocetrique | Prospective study | 6 | Lomboradiculalgies | 100% |
| Kloimstein[24]Austria-Switzerland multicetrique | Prospective study | 118 | Low back pain | 100% |
| Reverberi[12]USA monocetrique | Prospective study | 8 | Low back pain | 100% |
| Mac Roberts [25]USA monocetrique | Prospective study | 44 | Low back pain | 100% |
| Nantes seriesFrancemono-centrique | Retrospective study | 80 | Low back painLombosciatalgies | 50% |
Table 1: Fourteen studies published in the literature in the lumbar skin stimulation, Six prospective series, nine retrospective series.
Nantaise series showssimilar results with 73% improvement. In literature the stimulation parameters also vary. They range from 2.1 to 5.7 volts (3.8 V average) of 210-450 microseconds (average 278) and 50 to 90 Hz (54 Hz average). Drug treatment was reduced by 34% for all series. Complications are low in the order of 2.6% in the literature and include electrode migration, infection or skin erosions.
Discussion
The absence of serious adverse events involved in the acceptance of the equipment, bit annoying for most patients and not painful. The compact nature of the equipment and its compatibility with the activities of daily life are contrasted with the technique of TENS sometimes effective but incompatible with an active lifestyle. The decrease in pain intensity contributes to the functional improvement and sometimes resumption of a professional activity, and decreased consumption of analgesics and co-analgesics, including opioids participates in the disappearance of certain side effects heavy, the overall improvement of the quality of life. Finally, we can mention the effect “dose” described by McQuay for TENS. The studies showed in fact an improvement of the effect over time of the sessions, the intensity and the total time from the beginning of the use of TENS [22-25].
All patients in this study had received upstream of TENS with greater than 50% efficiency. However none have met this technique over the long term for the following reasons: the electrodes can result in phenomena of skin allergies, excessive sweating causes the separation of the electrodes finally flooding of device makes it easily compatible with life active. The study of Falco [20] showed that 14 of 18 patients receiving subcutaneous stimulation had not previously taken benefit of TENS. The right response to TENS could be a positive predictive value of subcutaneous stimulation but not a negative predictive value. The link between these two techniques, including predictive character of TENS should be the subject of a separate study.
The absence of serious adverse event, the good tolerance of the surgical technique, reversibility and effectiveness corroborate the results from the international literature. We believe relevant to propose earlier subcutaneous nerve stimulation technique in the surgical management of chronic low back pain, especially when they have a good response to TENS.
Conclusion
The subcutaneous stimulation has significant efficacy for the treatment of chronic low back pain refractory to predominantly neuropathic component. The subcutaneous stimulation enhances all of the patients, sometimes with a total pain relief. The efficiency remains good even improve over the long term. Finally, the absence of serious adverse events and its minimally invasive character make a reliable technique. Thus, the subcutaneous lumbar stimulation could become a surgical treatment of first intension under chronic low back pain refractory to predominantly neuropathic component already having a good response to non-invasive neurostimulation technics.
References
- Attal N, Perrot S, Fermanian J, Bouhassira D (2011) The neuropathic components of chronic low back pain: a prospective multicenter study using the DN4 Questionnaire. J Pain 12: 1080-1087.
- Beith ID, Kemp A, Kenyon J, Prout M, Chestnut TJ (2011) Identifying neuropathic back and leg pain: a cross-sectional study. Pain 152: 1511-1516.
- Buchmuller A, Navez M, Milletre-Bernardin M, Pouplin S, Presles E, et al. (2012) Value of TENS for relief of chronic low back pain with or without radicular pain. Eur J Pain 16: 656-665.
- Baron D, Mimassi N (2013) Les lombalgies chroniques font le lit des douleursneuropathiques
- Paicius RM, Bernstein CA, Lempert-Cohen C (2006) Peripheral nerve field stimulation in chronic abdominal pain. Pain Physician 9: 261-266.
- Lipov EG, Joshi JR, Sanders S, Slavin KV (2009) Use of Peripheral Subcutaneous Field Stimulation for the Treatment of Axial Neck Pain: A Case Report. NeuromodulationTechnol Neural Interface 12: 292-295.
- Falco FJ, Berger J, Vrable A, Onyewu O, Zhu J (2009) Cross talk: a new method for peripheral nerve stimulation. An observational report with cadaveric verification. Pain Physician 12: 965-983.
- Nizard J, Raoul S, Nguyen JP, Lefaucheur JP (2012) Invasive stimulation therapies for the treatment of refractory pain. Discov Med 14: 237-246.
- Sharan A, Cameron T, Barolat G (2002) Evolving patterns of spinal cord stimulation in patients implanted for intractable low back and leg pain. Neuromodulation 5: 167-179.
- Oakley JC (2006) Spinal Cord Stimulation in Axial Low Back Pain: Solving the Dilemma. Pain Med 7: S58-S63.
- Navarro RM, Vercimak DC (2012) Triangular stimulation method utilizing combination spinal cord stimulation with peripheral subcutaneous field stimulation for chronic pain patients: a retrospective study. Neuromodulation 15:124-131.
- Reverberi C, Dario A, Barolat G (2013) Spinal cord stimulation (SCS) in conjunction with peripheral nerve field stimulation (PNfS) for the treatment of complex pain in failed back surgery syndrome (FBSS). Neuromodulation 16: 78-82.
- Hamm-Faber TE, Aukes HA, de Loos F, Gültuna I (2012) Subcutaneous stimulation as an additional therapy to spinal cord stimulation for the treatment of lower limb pain and/or back pain: a feasibility study. Neuromodulation 15: 108-116.
- Mironer YE, Hutcheson JK, Satterthwaite JR, LaTourette PC (2011) Prospective, two-part study of the interaction between spinal cord stimulation and peripheral nerve field stimulation in patients with low back pain: development of a new spinal-peripheral neurostimulation method. Neuromodulation J IntNeuromodulationSoc 14:151-154
- Verrills P, Vivian D, Mitchell B, Barnard A (2011) Peripheral nerve field stimulation for chronic pain: 100 cases and review of the literature. Pain Med 12: 1395-1405.
- Paicius RM, Bernstein CA, Lempert-Cohen C (2007) Peripheral Nerve Field Stimulation for the Treatment of Chronic Low Back Pain: Preliminary Results of Long-Term Follow-up: A Case Series. Neuromodulation 10: 279-290.
- Yakovlev AE, Resch BE, Yakovleva VE (2011) Peripheral nerve field stimulation in the treatment of postlaminectomy syndrome after multilevel spinal surgeries. J IntNeuromodulationSoc 14: 534-538
- Verrills P, Mitchell B, Vivian D, Sinclair C (2009) Peripheral nerve stimulation: a treatment for chronic low back pain and failed back surgery syndrome? Neuromodulation 12: 68-75.
- Burgher AH, Huntoon MA, Turley TW, Doust MW, Stearns LJ (2012) Subcutaneous peripheral nerve stimulation with inter-lead stimulation for axial neck and low back pain: case series and review of the literature. Neuromodulation 15: 100-106.
- Robert R, Raoul S, Hamel O, Doe K, Lanoiselée JM, et al. (2004) Chronic lower back pain: a new therapeutic approach. Neurochirurgie 50: 117-122.
- Ordia J , Vaisman J (2009) subcutaneous peripheral nerve stimulation with paddle lead for treatment of low back pain: case report. Neuromodulation 12: 205-209.
- Sator-Katzenschlager S, Fiala K, Kress HG, Kofler A, Neuhold J, et al. (2010) Subcutaneous target stimulation (STS) in chronic noncancer pain: a nationwide retrospective study. Pain Pract 10: 279-286.
- Kloimstein H, Likar R, Kern M, Neuhold J, Cada M, et al. (2014) Peripheral Nerve Field Stimulation (PNFS) in Chronic Low Back Pain: A Prospective Multicenter study. Neuromodulation 17:180-187.
- Jang JS, Choi HJ, Kang SH, Yang JS, Lee JJ, et al. (2013) Effect of pulsed radiofrequency neuromodulation on clinical improvements in the patients of chronic intractable shoulder pain. J Korean NeurosurgSoc 54: 507-510.
- McRoberts WP, Wolkowitz R, Meyer DJ, Lipov E, Joshi J, et al. (2013) Peripheral nerve field stimulation for the management of localized chronic intractable back pain: results from a randomized controlled study. Neuromodulation 16: 565-575.
- McQuay HJ, Moore RA, Eccleston C, Morley S, Williams AC (1997) Systematic review of outpatient services for chronic pain control. Health Technol Assess 1: 1-135.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 12654
- [From(publication date):
specialissue-2016 - Aug 25, 2025] - Breakdown by view type
- HTML page views : 11610
- PDF downloads : 1044