Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
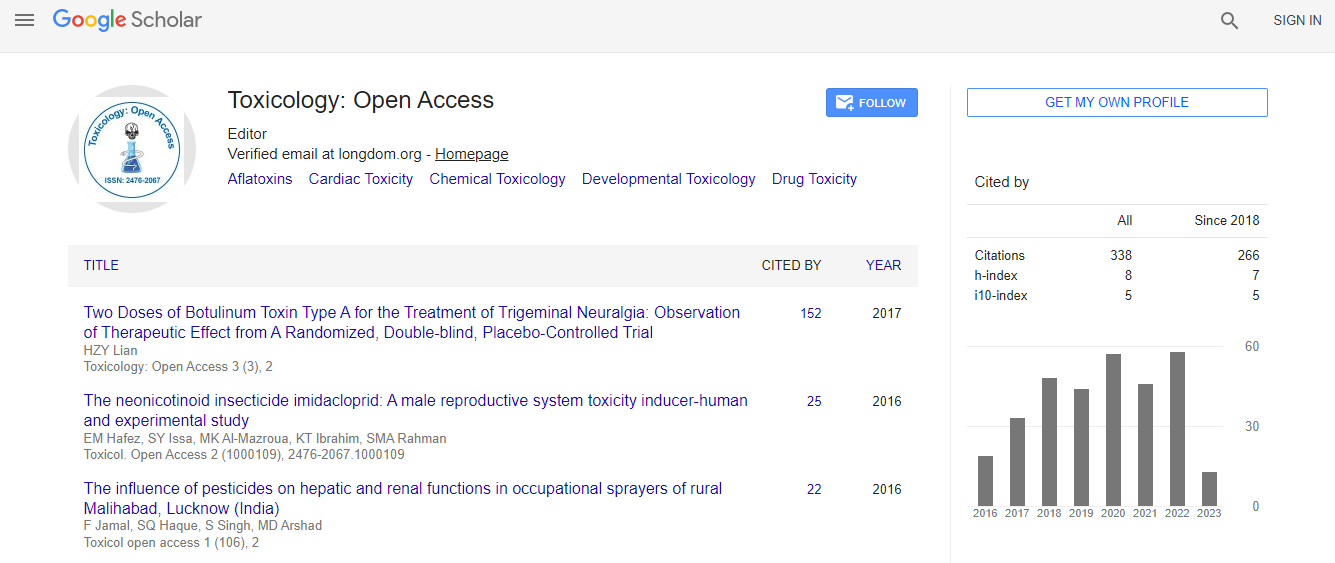
Google Scholar citation report
Citations : 336
Toxicology: Open Access received 336 citations as per Google Scholar report
Indexed In
- Google Scholar
- RefSeek
- Hamdard University
- EBSCO A-Z
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Related Subjects
Share This Page
Drug-induced hyperammonemia: Are there specific therapies?
8th World Congress on Toxicology and Pharmacology
Florian Eyer
Technical University of Munich, Germany
Posters & Accepted Abstracts: Toxicol Open Access
Abstract
Objective: The objective of this study was to give an overview about drugs capable to induce hyperammonemia (HA), to discuss their pathophysiology and to provide treatment options for HA. Methods: Literature review on PubMed and common textbooks. Results: Valproate (VPA) frequently induces HA, even if not overdosed. VPA and its metabolites inhibit enzymes of mitochondrial Ã?Â?-oxidation, which may cause depletion of carnitine and lower acetyl-CoA, essential for the synthesis of N-acetylglutamate (NAG). The latter is an allosteric co-factor of carbamoyl-phosphate-I-synthase, ultimately impairing detoxification of ammonia. Topiramate, Carbamazepine, Barbiturates, Salicylates may each contribute to HA, whereby underlying pathomechanisms are largely speculative or unknown. Finally, acetaminophen as the parent drug has been demonstrated to induce decreased activity of both, carbamoyl-phosphate-synthase-I and glutamine synthase. This was accompanied by HA indicating that CPS-I and/or glutamine synthase were inhibited in vivo to an extent sufficient to compromise ammonia clearance. Chemotherapeutics (CTX) frequently induce HA either by reduction in the expression of glutamine synthase, carbamoyl-phosphate synthase, and ornithinetranscarbamylase. CTX also may lead to functional arginine deficiency secondary to increased catabolism. Treatment Options: Immediate withdrawl of the offending drug suspicious for HA should be followed. Oral rifaximine can reduce bacterial ammonia synthesis in the gut, lactulose enema can entrap ammonia and hemodialysis may serve as a rescue therapy. Sodium-benzoate or phenylbutyrate can reduce ammonia synthesis and eliminate glycine and glutamine. Adequate amounts of dextrose (e.g. a 10% dextrose solution) and fatty acids should be provided, while protein intake should be paused. More specific treatment options include L-carnitine in deficient patients or infusion of L-arginine in patients with VPA-overdose. Administration of carglumic acid may overcome proximal inhibition of enzymes of the urea cycle. Conclusion: Although infrequent, HA may be a severe medical condition occurring during therapeutic pharmacological treatment or drug overdose. Understanding the pathophysiology, general or more specific treatment options may become life-saving.Biography
Email: florian.eyer@tum.de

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi