Research Article Open Access
Short Term Medical Response in Haiti: Epidemiology and Model for Delivery of Care
Karla Prentiss1, Tyler Prentiss1, Thomas Zervos2, Shauna King1 and Marcus Zervos2,3*
1International Medical Relief (IMR), Denver, Colorado
2Wayne State University School of Medicine, Detroit, MI
3Henry Ford Health System, Detroit MI
- *Corresponding Author:
- Marcus Zervos
Division Head, Infectious Diseases
Medical Director, Infection Control
Henry Ford Health System, Detroit, MI
Tel: 313-916-2573
E-mail: mzervos1@hfhs.org
Received date: October 31, 2011; Accepted date: December 17, 2011; Published date: December 20, 2011
Citation: Prentiss K, Prentiss T, Zervos T, King S, Zervos M (2011) Short Term Medical Response in Haiti: Epidemiology and Model for Delivery of Care. Epidemiol S2:002. doi:10.4172/2161-1165.S2-002
Copyright: © 2011 Prentiss K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Epidemiology: Open Access
Abstract
On January 12, 2010 a 7.0 magnitude earthquake struck Haiti, with several subsequent aftershocks. It was estimated that 200,000 to 230,000 died, more than 300,000 were left wounded and 1 to 1.3 million left homeless. We describe an intervention bundle that includes acute medical care, and community education. There were 641 male and 1042 female patients seen over an 8 day period. Mean age was 24.6yrs (range 30d to 94 years). Thirty eight percent of patients were under the age of 18 yrs. All patients sought medical and 254 patients also sought dental care. The most common presenting complaints were fever which occurred in 304 patients. Most common disorders seen were gastrointestinal illness in 222 patients, respiratory illness in 169, eye dryness in 162, skin infection in 153, pain and malaise in 151 and vaginal symptoms including sexually transmitted diseases in 118 patients. Sixty five women sought medical attention for pregnancy or complications. Fifty eight percent of children had received polio immunization and 55 percent stated they slept with bed nets.
Introduction
On January 12, 2010 a 7.0 magnitude earthquake struck Haiti, with several subsequent aftershocks. It was estimated that 200,000 to 230,000 died, more than 300,000 were left wounded and 1 to 1.3 million left homeless [1]. Haiti is considered the poorest country in the Western hemisphere [2]. Before the earthquake, less than half of the 9.7 million Haitian population had clean water and 83% did not have access to adequate sanitation facilities. The damage and loss of life had a catastrophic impact on the function of its government, health care facilities, and rudimentary utilities [2]. Over the last several months from 2010 to 2011 an estimated 500,000 cases of cholera has compounded the medical impact resulting from the earthquake [3].
Much has been written about the initial medical response and continuing delivery of medical care by academic and governmental institutions [4-8]. There is less information on epidemiology of infection, diagnosis of infectious diseases without laboratory resources, and development of strategies for the early control and prevention of the spread of infectious diseases in a poor sanitary environment and in the acute clinical setting.
Our aim is to discuss the impact of an intervention bundle as a model for short-term medical mission work. Furthermore, we felt it would be valuable to present how these issues are addressed in an acute care clinic, the sustainable benefits to this approach and information collected from a point prevalence study of disorders seen to be used to further clarify epidemiology.
Methods
This report describes an acute care medical mission clinic model and data collected on infections and disorders seen during a medical mission trip organized by International Medical Relief (IMR) during the period July 2-10, 2011 in Haiti. IMR is a nonprofit organization that provides medical relief and care to under-served and vulnerable people around the world, organizing medical mission trips worldwide. It was founded on the belief that knowledge of basic health facts and access to medical relief and care should be shared by all nations, regions, and classes. One goal is to establish long-term relationships that allow teams to revisit each village multiple times over several years until the community can maintain its medical status independently. This is done through short-term medical mission trips where volunteers give their time and services for the medical relief of the developing world. Each visit brings progress and success in community wellness allowing succeeding medical mission trips to provide more technical care. International Medical Relief provides medical relief in areas where health care is limited or difficult to obtain and in disaster areas, their work includes some of the millions of people who have been excluded from healthcare systems worldwide. The trip goal was to contribute to the communities by improving the overall health, wellness and medical relief of the people and collect epidemiologic data.
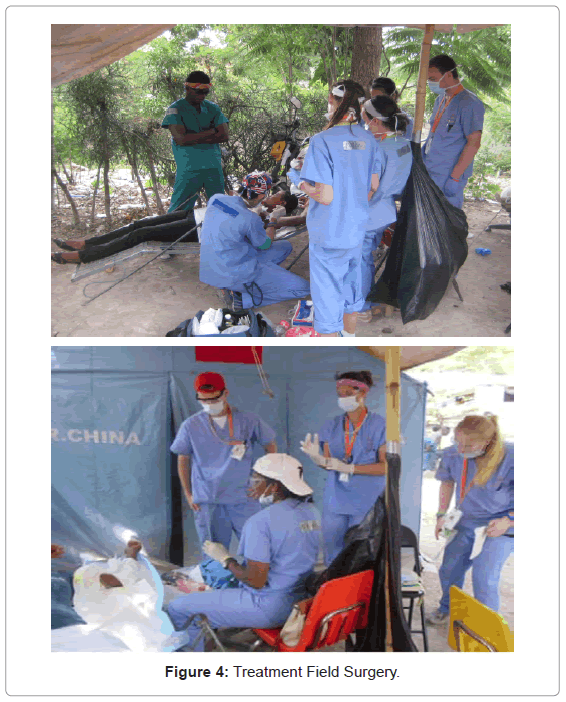
The medical team consisted of forty members including one overall team leader, one chief medical and one chief nursing officer. There was a diverse group of primary care providers including five physicians (surgeon, internist, infectious diseases, obstetrics and gynecology), three mid level providers (one family medicine physician assistant and two nurse practitioners, one each family medicine and pediatrics). There were three dentists (including one Haitian dentist), three nurses, three emergency medical technicians. The remainder of the team included United States medical students, post doctoral residents, community education workers, and Haitian medical students and nursing students.
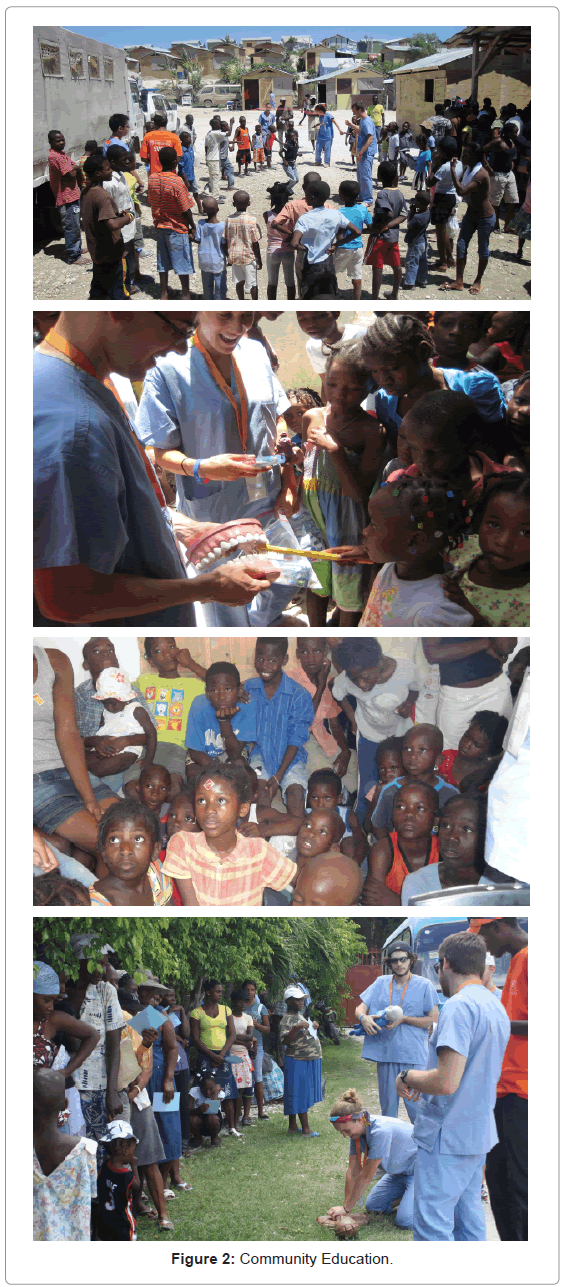
Community education projects included classes of 20 to 40 Haitians done in Creole, with written information provided, with the following topics included: basic first aid, CPR, SODIS and clean water, women’s health, children’s health, oral health, rehydration and prevention of cholera, prevention of malaria, prevention of diarrheal diseases, prevention of sexually transmitted diseases, with distribution of condoms, HIV prevention, disease prevention, diet and cholesterol management, trauma recovery, mental health awareness, nutrition, physical fitness, sexually transmitted diseases, menstrual cycle and family planning, skin infections and wound care, traffic and transportation safety, child safety, hygiene and sanitation, hand washing, alcohol and smoking cessation. Additionally, providers do one-on-one awareness and prevention training with patients at the provider stations.
Seven clinic locations in and around Port au Prince Haiti ware conducted. These included tent cities with internally displaced persons (IDPs) and rural locations particularly those most affected by the earthquake. The clinic was structured with intake, triage, wellcheck visits (including eye and physical exams), and surgical clinic including dental and wound care, the main provider area for diagnosis of treatment of diseases, pharmacy, and the community education stations. Patients needing examinations by medical providers were diagnosed and then sent to pharmacy. The initial dose of medication prescribed was administered in the clinic with a volunteer for to assure compliance and patient education. Information was collected on each patient on presenting complaint, diagnosis, treatment administered, use of bed nets, pregnancy (prior and current) status, number of children living, prior medical conditions and prior immunization status of themselves and children.
Results
Over the 8 day period there were 1696 patients seen. There were 641 male and 1042 female patients. Mean age was 24.6yrs (range 30d to 94 years). Thirty eight percent of patients were under the age of 18 yrs. All patients sought medical and 254 patients also sought dental care. All patients and providers participated in the community education sessions. Sixty five women sought medical attention for pregnancy or complications. The most common presenting complaints were fever which occurred in 304 patients. Gastrointestinal illness occurred in 222 patients, which included gastrointestinal reflux, parasitosis and acute diarrheal illness. Respiratory illness occurred in 169 patients who included mostly upper respiratory illness, pharyngitis and otitis in children. Eye dryness occurred in 162 patients, and was related to dust and smoke in the air. Skin rash including infections occurred in 153 patients; the infections included wound infection, cellultis, impetigo, ringworm and scabies. Pain and malaise occurred in 151 patients, and often related to former trauma. Vaginal symptoms related to fungal, bacterial vaginosis and likely sexually transmitted illness in 118 patients. Post traumatic stress related symptoms were common, often presenting as pain, vague abdominal complaints, anxiety and difficulty sleeping. Clinical presentations typical of tuberculosis, advanced AIDS, severe cholera were uncommon. Mumps was suspected in one patient, there were no cases felt to be measles or rubella. A summary of medical diagnoses are found in Table 1. Three patients were transferred to acute care hospitals, one for refractory seizures, a second for diarrhea refractory to oral rehydration likely secondary to cholera and the third for a large intra oral, retropharyngeal abscess.
| Diagnosis | Number of people (%) |
|---|---|
| Pain/headache | 317 (18.7) |
| Skin infection, scabies, ringworm, impetigo, cellulitis | 225 (13.3) |
| Vaginal Infection, candida, bacterial vaginosis | 157 (9.2) |
| Parasitosis (GI) | 143 (8.4) |
| Dehydration | 135(7.9) |
| Upper respiratory tract inf | 111 (6.5) |
| Dental extraction | 105 (6.2) |
| Gerd reflux | 103 (6.1) |
| Eye glasses/dry eyes | 95(5.6) |
| Urinary tract infection | 70 (4.1) |
| Pregnancy or complications | 65 (3.8) |
| Allergic rhinitis | 60 (3.5) |
| Well Child | 37 (2.2) |
| Gastroenteritis | 26 (1.5) |
| Otitis media | 17 (1.0) |
| STD, suspect chlamydia or gonorrhea | 16 (0.9) |
| Diabetic | 6 (0.3) |
| Lipoma | 3 (0.1) |
| Seizure | 2 (0.1) |
Table 1: Diagnoses of patients presenting to an acute care clinic in Haiti.
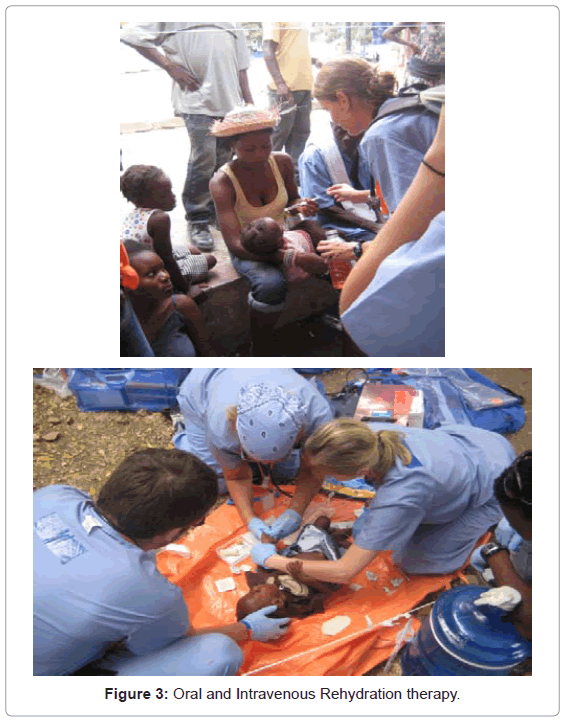
Eighty three percent of patients stated they had seen a provider in past, 16 percent previously diagnosis with a condition including malaria, TB or HIV, 45 percent had received prior immunization, 58 percent of children had received polio immunization and 55 percent stated they slept with bed nets. For women, number of pregnancies, live births and children currently were 3.38, 3.08 and 2.86 mean. The clinic set up, community education and surgical field used are shown in Figures 1-4.
Discussion
Hospitals and clinics in Haiti vary in size and design. Some of them, particularly shortly after the earthquake consisted of small tents, some dedicated to a specific type of care provided. Some hospitals were either structured as large tents or organized within buildings that previously functioned as hospitals, churches, or schools. Additionally, lack of running water was a common problem in most centers. Medishare, which was a collaborative effort between University of Miami and Jackson Memorial hospital in Miami and the Israeli field hospital, and IMR, were models for acute care hospital organization and were operational a few days after the earthquake [5-8] IMR was on the ground 6 days after the earthquake with providers working at Medishare, General Hospital, Adventist Hospital conducting orthopedic and plastic surgeries, urgent major wound care, as well as sending out teams into the IDP camps that were growing by the thousands every day, providing needs on site, including follow up care.
In the present study we report an intervention bundle that includes acute medical and dental care and community education. We found that fever was the most common presenting complaint, and the most common diagnoses were pain, skin infection, and gastrointestinal infection or reflux. Pregnancy was not common, and was present in 6.2% of women seeking clinic care. Importantly, bed nets were used in 55% of patients, which is higher than reported in earlier studies. A history of immunizations occurred in only 45 percent of the overall population, and polio immunization occurring in 58 percent of children. Although cholera has been reported to be common in Haiti diarrhea not responsive to oral rehydration was rare. The ability to provide antibiotics and oral rehydration therapy at early signs of infection were lifesaving.
The clinic was structured to include triage and data collection, medical, dental and wound care, well check exams, community education and pharmacy. All patients that sought medical care were seen, however patients were triaged between providers when that would improve patient care. At clinic triage, patients were screened for chronic cough or other potentially transmissible illness. If cough was present for over 2 weeks, masks worn by the patient was instituted [9]. Patients were also screened for diarrhea and if present, standard precautions used for handling of body fluids. Prior to the earthquake, tuberculosis constituted the seventh cause of death in Haiti, accounting for 4.7% of deaths among young adults [2]. Therefore masks were placed on patients with chronic cough. Personnel were instructed to wear N-95 respirators while caring for these patients. Arrangements were subsequently made for patients with suspicion of tuberculosis to be seen at a functioning hospital or clinic in the Port-au-Prince area that could do radiography or specialized in tuberculosis. A family member generally accompanied patients seeking medical attention. Families played an important role in assisting with follow up and medication adherence. Family members helped patients with rehydration. Hand disinfection was accomplished with alcohol hand sanitizer (ranging from 62% to 65% ethyl alcohol). These alcohol containers were placed in different areas within patient-care areas. Patients, family members, non-medical volunteers, and medical personnel were instructed to use hand sanitizer before and after patient care, before food manipulation, and following the use of toilets. Patients were also given community education on proper hand sanitation without sanitizer by vigorous rubbing of hands with clean water and proper nail clipping. Small table-top sterilizers were used for sterilization of instruments in clinic.
Although much has been written about the value of medical emergency response and projects that are long term and sustainable, the value of short-term medical mission has received less attention. The benefits can be summarized to include collection of statistical data, education of patients and providers, acute care provided that otherwise would not be available, provision of resources and new knowledge. The results of the present study provide an accurate assessment of the total community health. Within the communities treated, we encountered on average over 90 percent of the entire population of the immediate community. Even housebound patients were given house calls so the immobile are also captured in our health statistics. Government run census’ are the next closest assessment of data capture for a community. These data are often limited by not being conducted by medical professionals. The present study captured important and valuable data on patient healthcare statistics, particularly in more remote areas such as rural areas and tent camps. This information is critical for future work and design of intervention strategies. Having a majority of the community present for short-term clinics also provides unprecedented access to vaccinate the community.
The present intervention bundle provided an unparalleled ability to provide awareness and education to communities. Patients participated in the program because it was exciting to be a part of the event, and involved the entire community. Herein, we were able to train and educate both ill and well patients on important topics identified by our team that relate to the overall health and wellness of people in their community. The topics ranged from basic first aid, how to identify and treat common illnesses, prevention techniques for infectious diseases, living with chronic conditions, SODIS clean water and proper sanitation. When patients were diagnosed with an illness the treatment protocols included education on prevention and awareness prior to getting their medicine. This has proven to be an effective as return visits show fewer cases of illnesses previously presented.
Importantly, the clinic provided needed preventive services and identified treated conditions where interventions resulted in lives saved. Patients came into clinic that had diseases that without antibiotics for example can be life threatening. Patients also came to the clinic that otherwise would not have access to a clinic setting, and seek care only after too ill for effective intervention. Some of the clinic locations were remote where otherwise health services are inaccessible for the population. Still others in communities with clinics did not understand how to access their healthcare systems. In these instances, education on how to access their health system as well as where to go for treatment of chronic conditions took place.
Provision of resources was also accomplished by explaining to patients how to access their health systems. Identified were a number of chronic conditions that resulted in providing information on where care and medicines were available. Often those that presented with chronic conditions did not know how to get treatment for their condition. The clinic not only provided a diagnosis and treatment, but also information on their illness, how to live with the condition, and where to go and how to access the health care system. The mutual exchange of knowledge more often than not allowed the international provider insights towards newer methods, gifts of medical supplies or tools to ease daily work, and collaboration where doors can be opened for long term telemedicine or triage of surgical cases to larger more equipped facilities. We provided medical education and tools to community health workers so that these communities were left with resources to improve long-term health. In communities where healthcare workers do not exist we helped community leaders to identify candidates that our providers can train and give accommodation and tools to carry on with basic medical aid in the absence of a team.
The short term nature of this trip provided an opportunity for medical staff that is still actively practicing in their respective fields ability care for a very underserved population without having to take a sabbatical from their practice in order to participate. The trip allowed for the providers to take limited time away for the opportunity to serve. The clinics we conducted had very large turnouts. Standing clinics typically have a very small patient turnout on a daily basis and the patients’ conditions are limited in scope and not representative of the community as a whole. There is a substantial benefit to the providers and their patients in developed nations with new and enhanced medical knowledge and skills of the providers who participate.
Conclusion
Immediately after the January 12, 2010 earthquake that struck Port au Prince, Haiti, multiple teams from around the world responded to provide medical assistance to the thousands of injured Haitians. The intervention bundle described in this report of an acute care medical mission was staffed entirely by short term volunteers many with limited experience in the work of a field clinic. That said, the intervention team described has expertise at short-term medical missions and setting up temporary clinic sites with a proper medical structure, proper pharmacy, proper licensures and approvals, medical insurance, ground logistics of promoting clinic, obtaining drivers, interpreters, security and crowd control. Medically they operate similar to an outpatient facility in the US; and therefore are able to capitalize on the providers’ abilities and help the Haitians. The clinic operated as if they were treating their own patients in the US. This gives confidence to the providers allowing them to focus on what they do best, provide care to the patients. While many teams went in initially after the earthquake, the clinic philosophy was that of ‘first in – last out’. The disaster relief interventions included a tiered structure to the reaction of the disaster sending in immediate surgical and trauma teams with an emphasis on wound care and clean water access, followed up with general medical, dental, and PTSD teams with components of education and provision of acute care. Multiple treatment and infection control issues were encountered, and data collected that will be of use for future interventions. The challenges are likely common to those encountered by the acute care clinic setting and the experiences are worth sharing. Here we have described snapshots of the issues faced, and data collected organization of the acute care clinic that provides sustained benefit to the community, and how the staff coped to provide safe environments in very difficult situations.
Acknowledgements
All authors declare no financial support or conflict of interests pertaining to this article. Shauna King is president and founder of IMR.
References
- PAHO/WHO collaborating center (2010) Situation in Haiti - Report prepared by the University of Yale/New Haven.
- PAHO (2007) Health in the Americas. PAHO Scientific Publications, USA.
- De Cock KM, Centers for Disease Control and Prevention (CDC) (2011) Trends in global health and CDC's international role, 1961-2011. MMWR Surveill Summ 60: 104-111.
- Ginzburg E, O'Neill WW, Goldschmidt-Clermont PJ, de Marchena E, Pust D, et al. (2010) Rapid medical relief--Project Medishare and the Haitian earthquake. N Engl J Med 362: e31.
- Sullivan SM, McDonald KW (2006) Post-Hurricane Katrina Infection Control Challenges and the Public Health Role at a Mobile Field Hospital. Am J Infect Control 34: E11-E12.
- Merin O, Ash N, Levy G, Schwaber MJ, Kreiss Y (2010) The Israeli field hospital in Haiti--ethical dilemmas in early disaster response. N Engl J Med 362: e38.
- Kreiss Y, Merin O, Peleg K, Levy G, Vinker S, et al. (2010) Early disaster response in Haiti: the Israeli field hospital experience. Ann Intern Med 153: 45-48.
- Lichtenberger P, Miskin IN, Dickinson G, Schwaber MJ, Ankol OE, et al. (2010) Infection control in field hospitals after a natural disaster: lessons learned after the 2010 earthquake in Haiti. Infect Control Hosp Epidemiol 31: 951-957.
- Centers for Disease Control and Prevention (2010) Guidance for Relief Workers and Others Traveling to Haiti for Earthquake Response.
Relevant Topics
- Behavioral epidemiology
- Cancer epidemiology
- Disambiguation
- Economic epidemiology
- Emerging Infection
- Environmental epidemiology
- Epidemiology and Biostatistics
- Epidemiology and community health
- Epidemiology and disease control
- Epidemiology and infection
- Epidemiology of tuberculosis
- Etiology
- Genetic epidemiology
- Global Health
- HIV surveillance
- Intestinal epidemiology
- Nutrition epidemiology
- Oral/dental epidemiology
- Pediatric epidemiology
- Primary care epidemiology
- Renal epidemiology
- Reproductive Epidemiology
- Trends in maternal mortality
- Veterinary epidemiology
Recommended Journals
Article Tools
Article Usage
- Total views: 13372
- [From(publication date):
January-2012 - Oct 20, 2025] - Breakdown by view type
- HTML page views : 8877
- PDF downloads : 4495