Review Article Open Access
Bone Health in Metabolic Endotoxemia Related Obesity
Aliya IS1, Norhazilah M1, Faruk RM1, Amanov M1, Mariam IU1, Zainab M3, Gotam K2, Nordin S1 and Atif AB1*1Faculty of Medicine and Health Sciences, Universiti Sultan Zainal Abidin
2Faculty of Medicine, UCSI, Kuala Terengganu, Malaysia
3Department of Microbiology & Molecular Genetics, University of the Punjab, Pakistan
- Corresponding Author:
- Atif AB
Faculty of Medicine
Universiti Sultan Zainal Abidin
Tel: +6096275587
E-mail: atifamin@unisza.edu.my
Received date: February 05, 2015; Accepted date: April 28, 2015; Published date: April 30, 2015
Citation: Aliya IS, Norhazilah M, Faruk RM, Amanov M, Mariam IU, et al. (2015) Bone Health in Metabolic Endotoxemia Related Obesity. Interdiscip J Microinflammation 3:129. doi:10.4172/2381-8727.1000129
Copyright: © 2015 Atif AB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at International Journal of Inflammation, Cancer and Integrative Therapy
Abstract
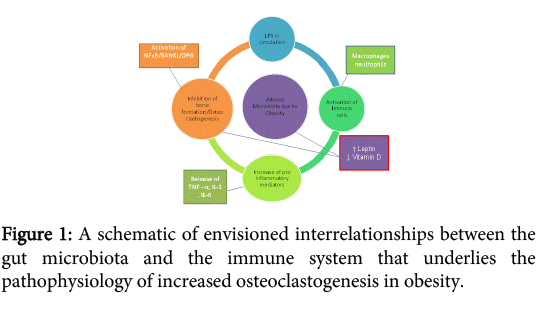
Obesity is a multifactorial disorder leading to multiple metabolic complications including hypertension, hypercholesterolemia, atherosclerosis, insulin resistance, type II diabetes and fatty liver. Recent research has discovered that obesity is associated with systemic low grade inflammation and one of the contributing factors can be alteration of gut microbiota due to change in dietary habits; attributed to high fat and carbohydrate diet. This altered microbiota brings along circulating lipopolysaccharide (LPS) which plays a key role in initiating low grade inflammation in adiposity associated with release of certain cytokines such as tumor necrosis factor (TNF) and interleukins especially interleukin1 (IL1) and marked by high C reactive protein, haptoglobulin alpha 1 acid glycoprotein (AAG) and alpha 1 antitrypsin (AAT) . In in this review we have focused on mechanism through which metabolic endotoxemia due to altered gut microbiome in obesity can also affect bone health and hinder bone formation. In addition to this exploring th possibility that increased leptin and decreased Vitamin D in obesity may supplement the bone loss.
Keywords
Metabolic endotoxemia; Lipopolysaccharides; obesity; Microbiota
Introduction
Obesity is a multifaceted malady which results as a consequence of imbalance between energy intake and expenditure. The pathophysiology of obesity involves intricate association with genetics, environmental factors, diet/caloric intake and lifestyle [1,2]. Recent research has shown that a low grade systemic inflammation is found in obese and this can be attributed to altered gut microbiota due to high fat and carbohydrate diet consumption at large [3]. This existence of low grade inflammation in obesity is marked by presence of elevated C reactive protein, haptoglobulin, alpha 1 acid glycoprotein (AAG) and alpha 1 antitrypsin (AAT) [4,5]. This can be the reason of widespread complications of obesity as inflammation persists systemically in the body.
The pathogenesis of cancer, aging, insulin resistance, atherosclerosis, pulmonary diseases, asthma, bowel disease, neurodegenerative disease and rheumatoid arthritis [6]; the conditions which can ascribed to obesity have involvement of inflammation as well. Moreover this low grade inflammation which is thought to be due to the lipopolysaccharides leakage into the circulation by the altered microflora , activate a series of mediators in immune system that can have systemic consequences [3]. This phenomenon of subclinically elevated levels of endotoxin in the bloodstream is known as “metabolic endotoxemia” [7,8]. In this review we focus on obesity related inflammation effecting bone metabolism and proposed mechanisms involved [9,10] moreover that Vitamin D deficiency and increased leptin in circulation can also augment the effects of LPS on bone.
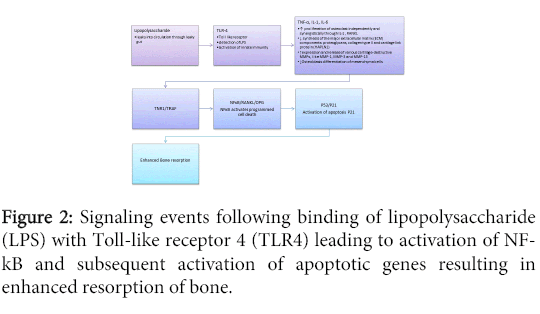
Considerable alterations in flora composition exist in obese animals and human subjects as compared to their leaner counterparts, showing a higher ratio of Firmicutes as compared to Bacteroidetes [11,12]. The reason for this alteration is due to improper dietary habits involving low consumption of fruits and vegetables, high intake of fats, insulinogenic foods, proteotoxins, gluten, zein [3,13] making individuals susceptible to dysfunctional microbiota, dysbiosis and chronic inflammation leading to increased production and leakage of endotoxins in the circulation [14]. The endotoxin or lipopolysaccharides (LPS) leaked into the circulation is basically immunogenic; it is present in the outer membrane of the gram negative bacteria [15]. The LPS induce proinflammatory molecules in the body such as Tumor necrosis factor (TNF), Interferon (INF), Interleukins (IL-1,IL-6, IL-8) [7,16,17].The pathogen-associated molecular pattern (PAMP) of LPS can then activate toll like receptors 4 (TLR-4) which belongs to the family of toll like receptors which are a type of pattern recognition receptors to identify pathogens foreign to host cell [18,19].
Bone is a dynamic tissue undergoing continuous remodelling that is bone formation and resorption and to maintain the constant bone mass the processes are equally balanced [20]. Bone comprise of 3 types of cells osteoblasts are the bone forming cells, osteoclasts acts as bone resorption cells and osteocytes are descendent of osteoblasts , play a crucial role in functional adaptation of bone by acting as mechanosensory cells [21,22]. Any disruption due to nutritional imbalance, infection or chronic illness hamper the healing process of wound and also affect fracture healing [23]. Obesity once reported to be protective against osteoporosis as [24] but with other studies it was seen that obesity may predispose to fracture susceptibility in obese [25,26].
Wahl and colleagues conducted a pilot study to see the effect of metabolic endotoxemia in mice model of osteogenesis distraction. Osteogenesis distraction (OD) is a surgical procedure in which the intrinsic capacity of bone to regenerate is being harnessed to lengthen bones or to replace large segments of bone in case of skeletal deformities. In this study low dose of LPS was injected in mice and detected upstream of TNF and reported impairment of bone repair in OD gaps radiologically and histologically concluding that LPS via increased TNF can impair bone repair [27]. However IL1 and IL-6- are also increased due to LPS and stimulate osteoclastogenesis [28].
TNF interacts with two types of receptors, termed TNF-R1 and TNF-R2. Most of TNF’s deleterious effects are channelled through TNF-R1. Many of the biologic properties of TNF overlap with those of IL-1. Both stimulate bone resorption by inducing the proliferation of osteoclast progenitors and, indirectly, by stimulating the resorbing activity of mature osteoclasts [29]. TNFα also activates osteoclasts both by themselves and in collaboration with receptor activator of NFkappa- B ligand (RANKL). RANKL exists both in a soluble and a membranous forms, which are controlled by 1,25-dihydroxyvitamin D3 and dexamethasone respectively [28]. Moreover, TNF-α levels are increased in synovial fliud, synovial membrane, subchondral bone and cartilage in patients with osteoarthritis. It functions through inhibition of synthesis of the major extracellular matrix (ECM) components and increase expression and release of various cartilage-destructive matrix metalloproteinases (MMPs). TNF-α acting through TNFR1 activates NFκB along with RANKL which in turn, regulates the expression of cytokines and so can maintain inflammatory reactions even if initial stimulus does not persist. It is suggested that NFκB acts via p53 and p21 which the apoptotic initiating factors leading to enhance resorption of bone.
In addition to this, obesity is also associated with vitamin D deficiency attributed to low physical activity and less exposure to sunlight of obese individuals [30,31], Vitamin D role is also established in immunomodulation which can lead to TLR4 activation and is also associated with its effects of inflammation plus secondary hyperparathyroidism can be found in obese due to sequestration of vitamin D in adipose tissue and excess excretion which can also lead to low bone density [32]. Hence the mechanism through which metabolic endotoxemia in obesity exerts negative effect on bone formation and repair is still challenging due to orchestrated and integrated actions of multiple factors which still have many loop holes to be filled up.
References
- Pérusse L, Chagnon YC, Bouchard C (1998) Etiology of massive obesity: role of genetic factors. World J Surg 22: 907-912.
- Redinger RN (2008) The prevalence and etiology of nongenetic obesity and associated disorders. South Med J 101: 395-399.
- Sulaiman I FR, Aliya IS, Adzim MKR, Uday YH Abdullah, Zahri MK, et al. (2014) Microbiota in Obesity. Interdiscip J Microinflammation 118.
- Maachi M, Piéroni L, Bruckert E, Jardel C, Fellahi S, et al. (2004) Systemic low-grade inflammation is related to both circulating and adipose tissue TNFalpha, leptin and IL-6 levels in obese women. Int J Obes Relat Metab Disord 28: 993-997.
- Trayhurn P, Wood IS (2004) Adipokines: inflammation and the pleiotropic role of white adipose tissue. Br J Nutr 92: 347-355.
- Maury E, Brichard SM (2010) Adipokine dysregulation, adipose tissue inflammation and metabolic syndrome. Mol Cell Endocrinol 314: 1-16.
- Hawkesworth S, Moore SE, Fulford AJ, Barclay GR, Darboe AA, et al. (2013) Evidence for metabolic endotoxemia in obese and diabetic Gambian women. Nutr Diabetes 3: e83.
- Chang S, Li L (2011) Metabolic endotoxemia: a novel concept in chronic disease pathology. J Med Sci 3: 191-209.
- Gower BA, Casazza K (2013) Divergent effects of obesity on bone health. J Clin Densitom 16: 450-454.
- SuÄur A, KataviÄ V, Kelava T, JajiÄ Z, KovaÄiÄ N, et al. (2014) Induction of osteoclast progenitors in inflammatory conditions: key to bone destruction in arthritis. Int Orthop 38: 1893-1903.
- Geurts L, Lazarevic V, Derrien M, Everard A, Van Roye M, et al. (2011) Altered gut microbiota and endocannabinoid system tone in obese and diabetic leptin-resistant mice: impact on apelin regulation in adipose tissue. See comment in PubMed Commons below Front Microbiol 2: 149.
- Musso G, Gambino R, Cassader M (2010) Obesity, diabetes, and gut microbiota: the hygiene hypothesis expanded? See comment in PubMed Commons below Diabetes Care 33: 2277-2284.
- Weickert MO, Pfeiffer AF (2008) Metabolic effects of dietary fiber consumption and prevention of diabetes. See comment in PubMed Commons below J Nutr 138: 439-442.
- Frazier TH, DiBaise JK, McClain CJ (2011) Gut microbiota, intestinal permeability, obesity-induced inflammation, and liver injury. See comment in PubMed Commons below JPEN J Parenter Enteral Nutr 35: 14S-20S.
- Beveridge TJ (1999) Structures of gram-negative cell walls and their derived membrane vesicles. See comment in PubMed Commons below J Bacteriol 181: 4725-4733.
- Zhang H, Peterson JW, Niesel DW, Klimpel GR (1997) Bacterial lipoprotein and lipopolysaccharide act synergistically to induce lethal shock and proinflammatory cytokine production. See comment in PubMed Commons below J Immunol 159: 4868-4878.
- Eggesb JB, Hjermann I, Lund PK, Joø GB, Ovstebø R, et al. (1994) LPSinduced release of IL-1 beta, IL-6, IL-8, TNF-alpha and sCD14 in whole blood and PBMC from persons with high or low levels of HDLlipoprotein. See comment in PubMed Commons below Cytokine 6: 521-529.
- Janssens S, Beyaert R (2003) Role of Toll-like receptors in pathogen recognition. See comment in PubMed Commons below Clin Microbiol Rev 16: 637-646.
- Rahman MM, McFadden G (2011) Modulation of NF-κB signalling by microbial pathogens. See comment in PubMed Commons below Nat Rev Microbiol 9: 291-306.
- de Baat P, Heijboer MP, de Baat C (2005) Development, physiology, and cell activity of bone. See comment in PubMed Commons below Ned Tijdschr Tandheelkd 112: 258-263.
- Aarden EM, Burger EH, Nijweide PJ (1994) Function of osteocytes in bone. See comment in PubMed Commons below J Cell Biochem 55: 287-299.
- Datta HK, Ng WF, Walker JA, Tuck SP, Varanasi SS (2008) The cell biology of bone metabolism. See comment in PubMed Commons below J Clin Pathol 61: 577-587.
- Gaston MS, Simpson AH (2007) Inhibition of fracture healing. See comment in PubMed Commons below J Bone Joint Surg Br 89: 1553-1560.
- Mendez JP (2012) Bone mineral density in postmenopausal Mexican- Mestizo women with normal body mass index, overweight, or obesity. Menopause.
- Kim KC, Shin DH, Lee SY, Im JA, Lee DC (2010) Relation between obesity and bone mineral density and vertebral fractures in Korean postmenopausal women. See comment in PubMed Commons below Yonsei Med J 51: 857-863.
- Cawsey S, Padwal R, Sharma AM, Wang X, Li S, et al. (2015) Women with severe obesity and relatively low bone mineral density haveincreased fracture risk. See comment in PubMed Commons below Osteoporos Int 26: 103-111.
- Wahl E (2012) Metabolic Endotoxemia and Inhibition of Direct Bone Regeneration: A Pilot Study. British Journal of Medicine & Medical Research 2: 510-519.
- Steeve KT (2004) IL-6, RANKL, TNF-alpha/IL-1: interrelations in bone resorption pathophysiology. Cytokine & growth factor reviews 15: 49-60.
- Assuma R, Oates T, Cochran D, Amar S, Graves DT (1998) IL-1 and TNF antagonists inhibit the inflammatory response and bone loss in experimental periodontitis. See comment in PubMed Commons below J Immunol 160: 403-409.
- Ahern T, Khattak A, O'Malley E, Dunlevy C, Kilbane M, et al. (2014) Association between vitamin D status and physical function in the severely obese. See comment in PubMed Commons below J Clin Endocrinol Metab 99: E1327-1331.
- Nair R, Maseeh A (2012) Vitamin D: The "sunshine" vitamin. See comment in PubMed Commons below J Pharmacol Pharmacother 3: 118-126.
- Lee P, Nair P, Eisman JA, Center JR (2009) Vitamin D deficiency in the intensive care unit: an invisible accomplice to morbidity and mortality? Intensive Care Med 35: 2028-2032.
Relevant Topics
Recommended Journals
- Journal of Lung Cancer Diagnosis & Treatment
- Advances in Cancer Prevention
- Breast Cancer: Current Research
- Cancer Surgery
- Immunology: Current Research
- Current Trend in Gynecologic Oncology
- Journal of Cancer Diagnosis
- Journal of Gastrointestinal Cancer and Stromal Tumors
- Cervical Cancer: Open Access
- Journal of Mucosal Immunology Research
- Journal of Oncology Research and Treatment
- Journal of Orthopedic Oncology
- Journal of Prostate Cancer
- Research and Reviews on Pathogens
Article Tools
Article Usage
- Total views: 12146
- [From(publication date):
July-2016 - Aug 18, 2025] - Breakdown by view type
- HTML page views : 11171
- PDF downloads : 975