Case Report Open Access
Case Report: Cerebral Toxoplasmosis Infection by Reactivation of T. gondii in Pediatric Patients with HIV
Marcela Espinoza-Oliva1, Erik Severiano Avila1, Maribel Barquera Artega1, Laura Veronica Sanchez Orozco2 and Maria de la Luz Galvan Ramirez2*
1UMAE, Hospital of Pediatrics, Western Medical Center, Mexican Social Security Institute, Mexico
2Department of Physiology, Neurophysiology Laboratory, Health Sciences University, Center, University of Guadalajara, Jalisco, Mexico
- *Corresponding Author:
- Maria de la Luz Galvan Ramirez
Department of Physiology, Neurophysiology
Laboratory, Health Sciences University, Center
University of Guadalajara, Jalisco, Mexico
Tel: 3310585313
E-mail: mlgalvanr@gmail.com
Received April 24, 2015; Accepted May 19, 2015; PublishedMay 22, 2015
Citation: Espinoza-Oliva M, Avila ES, Artega MB, Sanchez Orozco LV, Galvan Ramirez ML (2015) Case Report: Cerebral Toxoplasmosis Infection by Reactivation of T. gondii in Pediatric Patients with HIV. J Neuroinfect Dis 6:175. doi:
Copyright: © 2015 Espinoza-Oliva M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
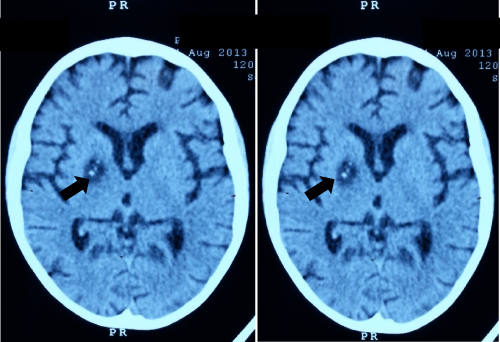
A neuro-toxoplasmosis was diagnosed in an HIV infected child stage AIDS C3. Case report: The patient coursed with recurrent respiratory infections, persistent cough with shortness of breath, fatigue, weakness, oral white plaques and fever predominantly at night up to 40°C. Mycobacterium tuberculosis was discarded. Then the patient had neurological impairment and Computerized Tomography (CT) scan of brain showed hyper dense images in the left sylvian aqueduct and in the right lenticular nucleus, the latter one with mixed concentric densities. Reactivation of toxoplasmosis was documented by high titers of IgG antibodies by Enzyme Linked Immunoabsorbent Assay (ELISA) corroborated by Western-blot.
Introduction
Toxoplasma gondii is causative agent of toxoplasmosis, in HIV carriers and AIDS patients, toxoplasmic encephalitis is the most frequent cause of focal brain lesions with a fatal outcome in these patients [1-3]. Toxoplasmosis reactivation is frequent when CD4 T-cells count (CD4) are <200/ml [4,5]. HIV-infected patients improve after starting Anti- Retroviral-Therapy (ART), due to ART reduce the HIV-RNA levels and boost the immune system. Nevertheless, in some patients, another response is seen after starting ART, this response is characterized by a clinical deterioration during immune recovery despite increased CD4 cell counts and decreased plasma HIV viral load; this phenomenon has been described as Immune Restoration Disease (IRD) or the Immune Reconstitution Inflammatory Syndrome (IRIS). During this syndrome is possible the reactivation of opportunistic infections because the immune system has an abnormal inflammatory reaction [6]. Immunity failure in HIV patients could explain the high prevalence of toxoplasmosis in these patients, being around 50-80% [7], in Mexico is about 42% however, in Jalisco state is 50.0% [8].
Case Report
Male patient, 9 years old, entered the service of Pediatric Infectious in the Western Medical Center, of Social Security on August 2013, the child was born and grown in a dysfunctional family with a mother with major depression. On admission, the child said that he suffered sexual abuse when he was 7 years old; the mother affirmed this. Six months before admission, the patient coursed with recurrent respiratory infections, persistent cough with shortness of breath, fatigue, weakness, oral white plaques and fever predominantly at night up to 40°C.
When arrived to hospital he had an Enzyme Liked Absorbent assay (ELISA) positive-HIV, he presented diarrheal stools during a week of evolution with hypovolaemic shock and fever, with warty skin lesion of 2 cm in left malar region, white patches on oral cavity, bradycardia, pulmonary hypoventilation, during palpation he had depressible soft abdomen in all four quadrants, absence of peritoneal irritation, intact limbs, increased tendon reflexes. Computerized Tomography of brain (CT scan) reported normal. The patient on admission showed clinical data characteristic of pneumonia and their parents reported a history of cough for more than 6 months of evolution. Search for alcohol acid resistant bacillus (AARB) in sputum and serial urine (3 samples), specific Mycobacterium tuberculosis culture and polymerase chain reaction (PCR) were performed. The patient received antimicrobial therapy transiently based on antifimic drugs: linezolid 20 mg kg/day, ciprofloxacin 30 mg kg/day, amikacin 15 mg kg/day intravenously.
The child presented acute renal failure, sinusal bradycardia, mild pericardial effusion and acute pancreatitis with lipase up to 5000 units/ dl, also Balthazar rated E by contrasted abdominal tomography. He received parenteral total nutrition (PTN), and then he improved with a final classification of Balthazar C.
Given the improvement observed in the pancreas, oral anti-tuberculosis drugs were adjusted; he received rifampicin 15 mg kg/day, isoniazid 10 mg kg/day, pyrazinamide 30 mg kg/day and ethambutol 15 mg kg/day; treatment that was suspended by negative reports of AARB and PCR for Mycobacterium tuberculosis. Positive anti HIV antibodies with titers of 65.3 UI/ml, viral load of 1,500,000 copies/ml; CD4 3/ ml. establishing the diagnosis of HIV/AIDS C3, vertical transmission was discarded. Fifteen days after admission, the child started antiretroviral treatment with zidovudine 460 mg/m2sc/day, Lamivudine 8 mg kg/day and Efavirenz 300 mg kg/day and profilaxis with Trimetropim sulfametaxazol. The patient had neurological impairment, hemiparesis in left hemisphere, chronic generalized tonic crisis and aphasia, cranial CT scan was performed, finding hyperdense images in the left sylvian aqueduct and in the right lenticular nucleus, the latter with mixed concentric densities (Figure 1).
Eighteen days after admission, results of laboratory tests: anticytomegalovirus antibodies were negative. Toxoplasma DNA negative by PCR in blood leukocytes, anti-Toxoplasma antibodies IgM negative by indirect ELISA (Platelia™ Toxo IgM 72841, Bio-Rad Marnes-la-Coquette France and Toxo IgG 72840) and IgG anti-Toxoplasma antibod- ies >300 IU/mL confirmed by Western-blot, settling down the diagnosis of cerebral toxoplasmosis. The child had contact with cats since he was 6 years old.
Treatment with Trimethoprim/Sulfamethoxazole was adjusted to 10 mg kg/day and clindamycin 40 mg kg/day intravenous. When the pancreatitis improved, the treatment with pyrimethamine and folic acid was started.
Twenty days later, presented clinical and hemodynamic deterioration; sustained hypothermia. Laboratory test: Hemoglobin 6.2 g/dL, lymphocytes 60%, neutrophils 10%, leukocytes 220 and platelets 22,000. The patient presented prolonging clotting times and thrombocytopenia, disseminated intravascular coagulation and multiple organ failure, with progressive deterioration despite treatment, suffering cardiac arrest and died twenty-one days after diagnosis of cerebral toxoplasmosis.
The lesions of brain toxoplasmosis can be unique or multiple, consequently the signs and symptoms are variable depending on the number, size and topography of these lesions. Due the most frequently localization of encephalitis lesions by Toxoplasma are in the corticalsubcortical binding of the cerebral hemispheres and basal ganglia, contralateral hemiparesis is the most common focal sign followed by ataxia, as was reported in this case.
CT scan initially was normal, after neurologic damage the CT showed focal lesion of basal ganglia on the right side below the head of the caudate nucleus dorso-ventral, latero-lateral as well as rostro-caudal respectively with central punctuate calcification. This type of injury has been reported in children with neurotoxoplasmosis (NT) [1,9], Neuroimaging changes may precede or follow of calcifications and microangiopathy in CT and/or white matter lesions and central atrophy on MRI. Cerebral Toxoplasmosis can be present in children with advanced stages of the disease [1,2,4]. This case was found in stage C3 and supported by high level of IgG antibodies confirmed by Western blot and the image studies TC suggested NT. The IgM anti-Toxoplasma was negative, because the illness represents a reactivation [8,9]. In this case, CD4 was very low (3 cells/ mm3), a significant association between NT and CD4 count <100 cells/mm3 has been reported [5,10]. A high risk to NT by reactivation of Toxoplasma was evidenced in this case by the high titers of IgG anti-Toxoplasma antibodies and by the clinical image findings. This case demonstrates the importance of IgG anti-Toxoplasma antibodies screening in all HIV positive patients. In case of positive results, patients must be treated in order to prevent reactivation of this infection that can be mortal when immunosuppression is severe. Another possibility was development of IRIS, this syndrome affects 10-25% of patients with AIDS and has been associated with a variety of infectious and noninfectious disease typically occurs within 60 days after start ART. Failure to recognize this disease has been responsible for additional hospitalizations and an increased number of invasive procedures [11]. Nevertheless, in this case we could not be able to asseverate if NT was a consequence of IRIS, since unfortunately the child died before to know if the HIV viral load decreased and if CD4+ cells increased after ART treatment. Living with cats requires an extreme sanitary control of the pets, particularly in immune compromised patients due to the high risk of toxoplasmosis transmission.
References
- Ibebuike K,Mantanga L, Emereole O, Ndolo P, Kajee A, et al. (2012) Cerebellar toxoplasmosis in HIV/AIDS infant: case report and review of the literature. NeurolSci 33: 1423-1428.
- Ramírez-Crescencio MA,Velásquez-Pérez L, Ramírez-Crescencio MA, Velásquez-Pérez L (2013) Epidemiology and trend of neurological diseases associated to HIV/AIDS. Experience of Mexican patients 1995-2009. ClinNeurolNeurosurg 115: 1322-1325.
- Ganiem AR, Dian S, Indriati A, Chaidir L, Wisaksana R, et al. (2013) Toxoplasmosis Mimicking Subacute Meningitis in HIV-Infected Patients; a Cohort Study from Indonesia. PLoSNegl Trop Dis 7: e1994.
- Mitchell W1 (2001) Neurological and developmental effects of HIV and AIDS in children and adolescents. Ment Retard DevDisabil Res Rev 7: 211-216.
- Walle F,Kebede N, Tsegaye A, Kassa T (2013) Seroprevalence and risk factors for Toxoplasmosis in HIV infected and non-infected individuals in Bahir Dar, Northwest Ethiopia. Parasit Vectors 6: 15.
- Achappa B,Madi D, Shetty N, Mahalingam S (2012) A Patient with Multiple Immune Reconstitution Inflammatory Syndrome (IRIS) Following Initiation of Antiretroviral Therapy. J ClinDiagn Res 6: 1547-1549.
- Grant IH, Gold JW, Rosenblum M, Niedzwiecki D, Armstrong D (1990) Toxoplasma gondii serology in HIV-infected patients: the development of central nervous system toxoplasmosis in AIDS. AIDS 4: 519-521.
- GalvánRamírez ML, Valdez Alvarado V, Vargas Gutierrez G, Jiménez González O, GarcíaCosio C, et al. (1997) Prevalence of IgG and IgM anti-Toxoplasma antibodies in patients with HIV and acquired immunodeficiency syndrome (AIDS). Rev Soc Bras Med Trop 30: 465-7.
- Drut R, Anderson V, Greco MA, Gutiérrez C, de León-Bojorge B, et al. (1997) Opportunistic infections in pediatric HIV infection: a study of 74 autopsy cases from Latin America. The Latin American AIDS Pathology Study Group.PediatrPathol Lab Med 17:569-76.
- Doraiswamy V,Vaswani RK, Lahiri KR, Kondekar SS (2010) Neurotoxoplasmosis mimicking intracranial tuberculoma. J Postgrad Med 56: 31-34.
- Chen KC, Chen JY, Tung GA (2009) Case 149: Immune reconstitution inflammatory syndrome. Radiology 252: 924-928.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 16716
- [From(publication date):
May-2015 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 11993
- PDF downloads : 4723