Research Article Open Access
Effects of Self-efficacy on Health Behavior and Body Weight
Faghri P1*, Simon J1, Huedo-Medina T1 and Gorin A21Department of Allied Health Sciences, University of Connecticut, Storrs, Connecticut, USA
2Department of Psychology, University of Connecticut, Storrs, Connecticut, USA
- *Corresponding Author:
- Pouran D Faghri, MD
MS, FACSM, Director
University of Connecticut Center for Environmental Health and Health Promotion
University of Connecticut
358 Mansfield Road
U-2101 Koons Hall
Room 318, Storrs, Connecticut, USA
Tel: 860-486-0018
Fax: 860-486-5375
E-mail: Pouran.Faghri@uconn.edu
Received date: October 31, 2016; Accepted date: November 26, 2016; Published date: December 09, 2016
Citation: Faghri P, Simon J, Huedo-Medina T, Gorin A (2016) Effects of Self-efficacy on Health Behavior and Body Weight. J Obes Weight Loss Ther 6:329. doi: 10.4172/2165-7904.1000329
Copyright: © 2016 Faghri P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Obesity & Weight Loss Therapy
Abstract
Objective: Overweight and obesity is a major public health in the U.S. Self-efficacy plays a significant role in health behavior (exercise and diet) and lack of could contribute to obesity. Our purpose was to evaluate perceived self-efficacy as it relates to eating, exercise and BMI in individuals with overweight and obesity.
Methods: 99 employees from 4 nursing-homes in Northeast U.S. participated, all with a body mass index (BMI)>25.0 kg/m2. Eating and exercise self-efficacy (Eat-SE, Ex-SE), Healthy Eating Scores (HES), and physical activity (PA) were assessed using questionnaire responses. Correlation and mediation analysis examined the influence of Eat-SE and Ex-SE on PA, HES and BMI.
Results: Higher HES predicted higher Eat-SE (p=0.02) and in turn, a lower BMI (p=0.02). Increased frequencies of moderate and vigorous PA predicted higher Ex-SE (p=0.01, p=0.00). Moderate PA further predicted lower BMI (p=0.05). 44% of the total effect of vigorous PA on BMI was mediated by Ex-SE (p=0.01).
Conclusion(s): Our models combining self-efficacy and behavioral variables captured variations in BMI in overweight and obese individuals. Future obesity interventions should incorporate improvement in self-efficacy for overcoming barriers to weight management.
Keywords
Overweight; Obesity; Self efficacy; Diet; Exercise
Introduction
Obesity is a growing epidemic in the United States, with more than two-thirds of U.S. adults currently overweight or obese [1]. It is predicted that by 2030, 51% of the U.S. population will be obese (a 33% increase in obesity and 130% increase in severe obesity) [2]. Obesity leads to comorbidities such as Type 2 Diabetes, cardiovascular disease and hypertension, further contributing to increased morbidity, mortality and healthcare costs across the nation [3,4]. Obesity and its related health consequences are significant factors driving healthcare spending. In 2008, obesity-related medical care costs were estimated to have risen to $146 billion dollars per year, accounting for almost 10% of all medical spending [5]. If these trends continue, it is estimated that by 2030, the costs of obesity in the U.S. could reach up to 18% of all U.S. health expenditures annually [5]. The economic burden of obesity is not only a major public health concern for the U.S., but is also becoming a global health crisis [6]. There is a critical need to stop or slow the progression of this epidemic.
The obesity epidemic involves a complex interaction of biological, environmental, sociocultural, behavioral, cognitive, and motivational factors. Socio-environmental lifestyle patterns have shifted in recent years, contributing to an increased sedentary lifestyle. Improvements in technology has increased the prevalence of sedentary jobs to 83% since 1950, while physically active jobs make up less than 20% of the current workforce [5]. In addition, the average workweek is longer, with full time US workers averaging 47 hours of work per week, accounting for over 350 more hours of sedentary activity over the course of a year [5]. 40% of Americans also report no leisure time physical activity, which is for most people the greatest opportunity for affording exercise outside of normal daily routines [7]. Less than 4% of US adults meet the recommended minimum amounts of physical activity, and most consume well in excess of their caloric needs [8].
Increasing physical activity and improving healthy eating habits can lower the risk of obesity. Individuals with obesity who lose even relatively small amounts of weight are likely to experience health benefits, such as improvements in diabetes control, reduction of CVD risk factors, and improved psychosocial functioning [9,10]. It is well established that health behaviors, such as regular exercise, healthy dietary habits and maintaining an appropriate body weight, are associated with lower morbidity and mortality [11]. Despite this knowledge, most Americans fall short of such health behaviors.
Self-regulation of health behaviors involves many psychological and behavioral factors [12]. The ability to make positive lifestyle behavior changes is strongly rooted in intrinsic factors such as motivation, readiness to change, and confidence, all of which are involved in the construct of self-efficacy. Self-efficacy refers to an individual’s belief in his or her capacity to execute behaviors necessary to produce specific performance attainments [13]. An individual’s perceived self-efficacy reflects his or her confidence in their ability to exert control over their own behavior, motivation and environment. The amount of effort an individual is likely to invest towards achieving an outcome, despite challenges along the way, may be explained by the individuals’ perceived self-efficacy to regulate a behavior. Self-efficacy plays a strong role in individuals’ perceived skills, perceived barriers, and weight management practices, and is thought to be a central psychosocial factor underpinning weight management practices [14].
Previous research has shown self-efficacy to be a strong predictor of health behaviors and weight control, including physical activity and dietary intake [9,12]. Current research states that higher levels of selfefficacy in behaviors such as healthy eating and exercise have been associated with lower BMI [15] and improved health outcomes [7]. However, individuals with obesity tend to have less perceived selfefficacy regarding health behaviors [9] like exercise [7] and dietary intake [9,16]. Higher BMI is also associated with greater perceived barriers to physical activity implementation and maintenance [7]. Perceived barriers to obesity management are associated with lower levels of motivation and perceived ability to manage overweight and obesity in adults [14]. Overall, self-efficacy appears to be a major factor impacting health behaviors related to eating behaviors and physical activity therefore, body weight.
With the significant increases in the rate of obesity, it is pertinent to identify psychological factors that may affect health-related behaviors including dietary and physical activity habits and weight control. Identifying mediators in the relationship between health behaviors and BMI is a critical step in the process of facilitating positive lifestyle and behavior changes. There is a clear need to develop and examine methods to improve individuals’ beliefs in their ability to lose weight and maintain the weight loss, especially for those who are already overweight or obese. This could facilitate the weight loss process and increase likelihood of achieving and maintaining weight loss goals. More investigation is needed in identifying cognitive variables affecting health behavior, such as self-efficacy. The primary purpose of the present study was to evaluate the relationship between perceived self-efficacy, eating and exercise behaviors, and BMI in individuals with overweight and obesity who are at risk for Type 2 Diabetes.
Methods
Design
This study used a cross-sectional design using a self-report questionnaire. University institutional review board approval was granted and participants’ informed consent was obtained prior to data collection.
Sample
The study sample was 99 full or part-time employees at 4 long-term care facilities in the Northeastern United States who participated in a weight loss program. All of the participants were overweight or obese according to CDC recommendations (WHO, 2014), and were at risk for Type II Diabetes. Participants were required to be at least 18 years of age.
Measures
Participants completed a questionnaire to self-report their demographic information, and respond to questions regarding their health and health-related behaviors. Trained health educators measured participant height and weight to calculate BMI. A calibrated Seca 700 physician balance beam scale was used to measure weight to the nearest 0.1 kg and height was measured the nearest mm. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared and categorized based on CDC recommendations of overweight (25-29.99 kg/m2), obese class I (30-34.99 kg/m2), obese class II (35-39.99 kg/m2), and (>40 kg/m2).
To measure eating behavior, a frequency-based Healthy Eating Score (HES) consisted of nine questions was used. The HES asked respondents to answer how often on a 4-point Likert scale, they consume unhealthy foods (fried food, red meat, processed meat, oily food, high fat diary, and high fat sweets) and healthy foods (whole grains, fruits, vegetables). The Likert scale ranged from “never to <1 time/week (1), 1-4 times/week” (2), “5-7 times/week” (3), “2 times/ day” (4). The scores were reverse coded when needed. A one global scale was then generated with the highest possible score of 36 (9 × 4).
Eating self-efficacy (Eat-SE), was defined in terms of a summary score consisting of 20 questions, which asked participants to rate their confidence that they could motivate themselves to resist eating in certain situations, consistently, for at least six months. Rating was performed using a 4 point Likert-type scale, “not confident” (1), “somewhat confident” (2), “moderately confident” (3), and “very confident” (4). The situational factors consisted of: Negative Emotions (ex: eating when anxious/sad), Availability (ex: eating when food is readily available, such as at a party), Social Pressure (ex: eating food when others encourage eating), Physical Discomfort (eating when in pain or fatigued), and Positive Activities (ex: eating while watching television). The scale provides one global scale with the highest possible score of 80 (20 × 4). The confidence-based Exercise Self- Efficacy Score (Ex-SE), was defined in terms of a summary score consisting of 11 questions, which asked participants to rate their confidence that they could motivate themselves to keep up with certain exercise behaviors and activities consistently for at least six months. Rating was performed using a 4 point Likert-type scale, “not confident” (1), “somewhat confident” (2), “moderately confident” (3), and “very confident” (4). The scale provides one global scale with the highest possible score of 44 (11 × 4). These scales have been previously tested and show evidence of reliability and validity [17].
The frequency-based Physical Activity Scores were defined using three questions, which obtained information on self-reported performance of mild, moderate, or vigorous physical activity for a 30 minute a day during a typical 7 day week. Individuals were provided with intervals of days for responses, including: 0 days, 1-2 days, 3-4 days, or 5 days or more [18,19].
Analysis
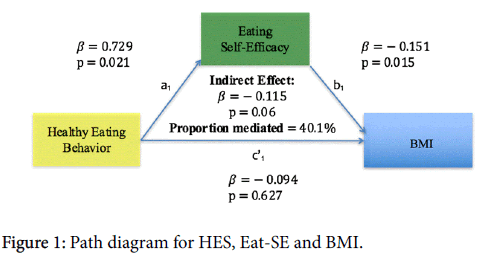
Frequency and means tests were run among different variables of the sample population using the Statistical Analysis Software program (SAS). These variables included gender, age, anthropometric measurements, race, and highest education level. Descriptive results were compiled and analyzed to assess overall population health, participant characteristics, distributions of variables of interest (selfefficacy, barriers to physical activity, obesity class). BMI normality was tested in SAS. Latent variables were created for HES, Eat-SE and Ex-SE using sum scores, where higher scores were indicative of a more healthful diet and higher perceived SE. Missing values were imputed using the Multivariate Imputation by Chained Equations (MICE) package in R. Bivariate correlations were run among variables in the Statistical Package for Social Sciences (SPSS). Mediation models were run in R Studio using the Mediation package (Figure 1).
Results
Sample demographics
The majority of participants were middle-aged females of white or black ethnicities with at least a high school diploma (12 years). All participants were overweight and obese, with the greatest number of participants classified in BMI Class 2 (Obese). Pearson’s correlation tests revealed that age had no significant correlation with BMI (r=0.022, p=0.837), eating self-efficacy (r=0.112, p=0.306), or exercise self-efficacy (r=-0.023, p=0.823). BMI normality followed a slightly non-normal distribution, as expected since all participants were overweight or obese. Table 1 shows Demographic analysis results.
| Gender | Male | 9.09% (n=9) |
| Female | 88.89% (n=88) | |
| Age | Years ± SD | 46.98 ± 11.36 |
| Anthropometrics | Weight (lbs) ± SD | 203.84 ± 40.93 |
| BMI ± SD | 35.33 ± 6.91 | |
| Weight Classification | Overweight | 19.79% |
| Obese | 34.38% | |
| Severe Obesity | 22.92% | |
| Morbid Obesity | 17.71% | |
| Super Obesity | 5.21% | |
| Race | White | 48.48% |
| Black | 40.00% | |
| Hispanic | 5.05% | |
| Asian | 3.03% | |
| American Indian | 1.01% | |
| Education | 10 yrs (high school/secondary) | 4.12% |
| 11 yrs (high school/secondary) | 3.09% | |
| 12 yrs (high school/secondary) | 40.21% | |
| 13 yrs (college/professional) | 12.37% | |
| 14 yrs (college/professional) | 12.37% | |
| 15 yrs (college/professional) | 10.31% | |
| 16 yrs (college/professional) | 10.31% | |
| 17 (post-graduate) | 7.22% |
Table 1: Demographic and anthropometric Variables (n=99).
General health, health behavior, and self-efficacy
The majority of participants reported their current general health as ‘good’ (45.8%), followed by ‘very good’ (28.1%), ‘fair’ (17.7%), and ‘excellent’ (7.3%). General health had a significant negative correlation with current level of physical activity (r=-0.284, p=0.006). General health also had a negative correlation with eating self-efficacy (r=-0.130, p=0.227) and exercise self-efficacy (r=-0.124), p=0.254), although not significant. Current level of physical activity was positively correlated with eating self-efficacy (r=0.268, p=0.011) and exercise self-efficacy (r=0.300, p=0.005). Physical activity was negatively correlated with BMI (r=-0.301, p=0.003). BMI was negatively correlated with moderate physical activity (r=-0.313, p=0.002) and vigorous physical activity (r=-0.233, p=0.026), as well as eating self-efficacy (r=-0.262, p=0.013) and exercise self-efficacy (r=-0.284), p=0.008). The top four reasons reported for not exercising include ‘never persisting’ (39.4%), ‘no time’ (32.3%), ‘lazy’ (28.3%), and ‘no energy’ (23.2%). Table 2 shows for Descriptive analysis results.
| General Health | Poor | 1.00% | Healthy Eating Score (max 36) | ||
| Fair | 17.20% | <20 | 9.50% | ||
| Good | 44.40% | 20-25 | 60.00% | ||
| Very Good | 27.30% | 26-30 | 26.00% | ||
| Excellent | 7.10% | >30 | 4.50% | ||
| Physical Activity | Mild | ||||
| 0 days | 24.20% | Self-Efficacy | |||
| 1-2 days | 36.40% | Eating | |||
| 3-4 days | 26.30% | Not Confident | 0.00% | ||
| ≥ 5 days | 11.10% | Somewhat Confident | 4.00% | ||
| Moderate | Moderately Confident | 32.30% | |||
| 0 days | 31.30% | Very Confident | 63.70% | ||
| 1-2 days | 39.40% | Exercise | |||
| 3-4 days | 19.20% | Not Confident | 0.00% | ||
| ≥ 5 days | 3.00% | Somewhat Confident | 13.00% | ||
| Vigorous | Moderately Confident | 42.40% | |||
| 0 days | 64.60% | Very Confident | 44.40% | ||
| 1-2 days | 18.20% | ||||
| 3-4 days | 9.10% | ||||
| ≥ 5 days | 1.00% | ||||
Table 2: Descriptive statistics (general health, health behavior, selfefficacy).
Mediation models
Higher Healthy Eating Score (HES) predicted higher Eat-SE (β=0.73, p=0.02) and higher Eat-SE further predicted a lower BMI (β=-0.15, p=0.02). Eat- SE marginally mediated the relation of HES on BMI, at 40% mediated (β=-0.115, p=0.06) (Figure 1).
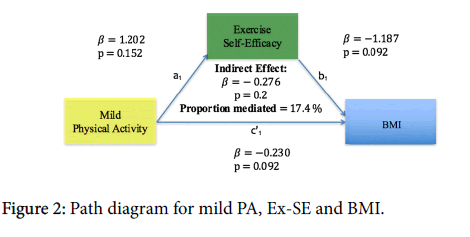
More frequent mild PA was associated with higher Ex-SE (β=1.2, p=0.15) and lower BMI (β=-0.23, p=0.09), and higher Ex-SE was associated with lower BMI (β=-1.19, p=0.09) (Figure 2).
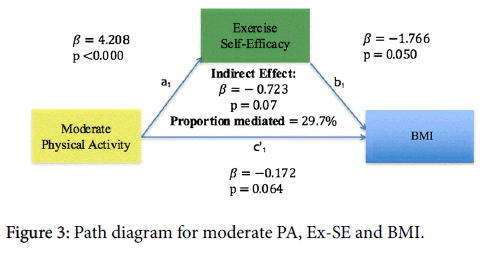
More frequent moderate PA predicted higher Ex-SE (β=4.2, p=0.00) and lower BMI (β=-0.17, p=0.06). Higher Ex-SE further predicted lower BMI (β=1.77, p=0.05). Thirty percent of the total effect of Moderate PA on BMI was mediated by Ex-SE, with marginal significance (β=-0.72, p=0.07) (Figure 3).
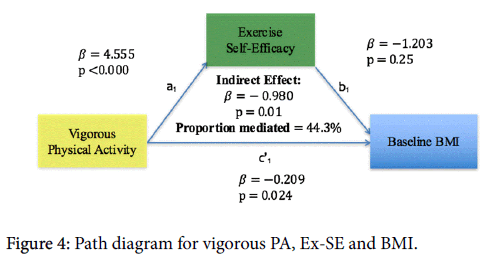
More frequent vigorous physical activity predicted higher exercise self-efficacy (β=4.56, p=0.00) and lower BMI (p=0.02). Forty four percent of the total effect of vigorous PA on BMI was significantly mediated by Ex-SE (β=-0.98, p=0.01) (Figure 4).
Discussion
Eating behavior
With the decline in diet quality in recent decades, the prevalence of Americans adults with overweight and obesity has risen to 69% [5]. In the present study, mediation analysis revealed that a higher healthy eating score was associated with higher eating self-efficacy (p=0.02), and a higher eating self-efficacy further predicted a lower BMI (p=0.02). Furthermore, self-efficacy was a marginally significant mediator of healthy eating score (40%, p=0.06). Previous studies have shown self-efficacy to be a strong predictor of dietary intake and weight control [9,12,20].
Inappropriate eating habits are common among women with Type 2 Diabetes and have been shown to be associated with lower self-efficacy for diet and exercise self-management, and higher BMI [21]. Poor eating habits are often viewed as negative contributors in weight control and are associated with more perceived barriers to weight loss [22].
Reasons for lower self-efficacy regarding eating healthy could also be due to socioeconomic factors, including education, job type, income, access to healthy foods, lack of cooking skills, and knowledge of eating healthy (such as benefits and what constitutes “healthy”). Our sample of nursing home employees are at lower socioeconomic status. Lower income has been recognized as a limiting factor in eating healthy, as foods high in calories, fats and sugars are generally more affordable [23]. Lower diet quality is reflected by lower consumption of vegetables, fruits and whole grains, and higher consumption of refined grains, fat and added sugars [24,25]. Individuals of a lower SES have been shown to have an elevated risk of developing chronic diseases such as Diabetes and CVD [24,25]. An increased dependence on westernized diets has largely contributed to weight gain and associated chronic diseases [26]. Higher healthy-eating self-efficacy have been23 associated with greater intention to make healthier food choices and participate in physical activity [26].
Exercise behavior
The American Heart Association (AHA) and the American College of Sports Medicine recommend at least thirty minutes of moderate activity (at least 5 days/week, or weekly total of 150 minutes) or at least twenty-five minutes of vigorous activity (at least 3 days/week, or a weekly total of 75 minutes) [5]. The 2008 Physical Activity Guidelines for Americans states that adults should engage in 2.5 hours of moderate or 1.25 hours of vigorous activity per week in order to achieve substantial health benefits, in addition to muscle-strengthening activities at least 2 days per week [27]. Examples of such intensity levels include brisk walking or gardening (moderate) to jogging or kickboxing (vigorous).
Our participants fell short of these recommendations. A majority of participants reported only 0-4 days of mild or moderate physical activity per week. 64.7% reported zero days of vigorous activity per week, while only 27.4% reported engaging in any vigorous physical activity at all. Current level of physical activity was significantly negatively correlated with general health (r=-0.284, p=0.006), which the majority of participants rated as ‘good’. The top four reasons reported for not exercising include: ‘never persisting’ (39.4%), ‘no time’ (32.3%), ‘lazy’ (28.3%), and ‘no energy’ (23.2%).
Gender-associated roles that have become the social-norm play an important role in women’s physical inactivity [28]. Several genderbased barriers to physical activity exist for women compared to men: less time to dedicate to regular exercise due to care-giver responsibilities; hobbies and leisure activities, which are typically less active than those of men; and women’s’ image-expectations in their community [28]. This may be one factor causing the study sample to be more physically inactive.
The present study reveals that more frequent moderate and vigorous physical activity is significantly predictive of higher exercise selfefficacy (p=0.00, p=0.00). These findings are consistent with previous studies which also found moderate and vigorous exercise to be positively influenced by intrinsic motivation and self-efficacy [29-31]. Mediation analysis also reveals that more frequent physical activity further predicted a lower BMI (p=0.05). Exercise self-efficacy was a significant mediator of vigorous physical activity on BMI, accounting for 44% of the total effect (p=0.01), and it was a marginally significant mediator of moderate physical activity (30%, p=0.07) on BMI.
Leisure time physical activity has been shown to be predicted by self-motivation, perceived barriers and benefits, and BMI. Exercisers are more likely to possess lower BMIs body mass values, possess higher self-motivation, perceive more benefits to exercise and perceive less barriers to exercise than non-exercisers [32]. A relatively small percentage of the present participants reported engaging in any vigorous activity (27%). Those who are vigorous exercisers, had the first-hand knowledge, experience and motivation to push themselves to exercise regularly, had higher self-efficacy to continue their exercise routines, believed they could perform future exercise behaviors (hence, the significant mediation effect seen of self-efficacy between vigorous activity and BMI).
Individuals with a strong sense of self-efficacy view challenges as something to be mastered. They developed deeper interest and commitment in activities in which they participate. Those with low self-efficacy often avoid tasks they find challenging (physical activity). There was a wide distribution of both physical activity levels and level of exercise self-efficacy for the majority of the sample, which may be why the models involving mild to moderate activity had more variability in mediation significance.
Cognitive factors such as stress, anxiety, depression and self-image can adversely affect self-efficacy and health behaviors. For example, some people perceive their excess weight as emotionally distressing, while others of similar weight are unaffected by it [33,34]. This could potentially deter participants with low self-efficacy from attempting to make changes, such as making time to go to the gym and/or initiating exercise. On the other hand, the adoption of exercise and engaging in regular physical activity is associated with decreased stress and anxiety, and improved mood and self-image, which can all improve one’s quality of life and facilitate the process of making healthier lifestyle choices. These changes could lessen perceived barriers and thus improve self-efficacy for performing activities. Exercise also may contribute to improved compliance with a healthy diet [35]. By learning how to minimize stress and elevate mood when faced with difficult or challenging tasks, individuals can improve their sense of self-efficacy and thus, achieve improved health behaviors and outcomes [13].
As the obesity epidemic continues to grow, so do the struggles of interventions combatting it. Recent research has provided evidence to suggest that cognitive factors, such as self-efficacy, play a major role in individual engagement of health behaviors. Findings from this study agree that self-efficacy is a promising factor affecting health behaviors, and could be a focus of improvement in future obesity interventions. Identifying mediators in the relationship between health behaviors and BMI is a critical step in the process of facilitating positive lifestyle and behavioral changes.
Cognitive and psychological factors interact with our physical environment in highly complex ways. There is a large heterogeneity in the way individuals physiologically and cognitively respond, which largely contributes to body mass and weight. All individuals with overweight and obesity are not the same, meaning a “one size fits all” approach is ineffective when attempting weight loss. It is inappropriate to assume that giving all individuals with obesity for example, the same treatment will produce similar outcomes [22]. Prior studies have indicated that factors such as personal preference, outcome expectancies, attitudes towards physical activity and exercise, body image, emotional distress and depression should be considered when determining appropriate treatment strategies [22].
Improving individuals’ perceived self-efficacy and belief in their ability to make healthful lifestyle changes would likely facilitate weight loss and desired health outcomes. The results of our study indicate that future interventions should focus on improving participants’ perceived self-efficacy to achieve greater weight loss. Educational interventions which recognize and address individuals’ perceived barriers and personal beliefs, and work to improve their readiness to change towards healthful behaviors, are more likely to achieve greater success in weight loss outcomes. Once individuals become more autonomous and self-motivated, they are more likely to successfully maintain weight status after weight loss. Laying a foundation of improved selfefficacy relating to health behaviors may be a pre-requisite for weight loss management.
Future interventions can also improve outcomes by first identifying other factors contributing to weight change, by examining alternative methods such as causal mediators of health behaviors affecting body weight for individuals who have lower self-efficacy and are less likely to succeed.
Limitations
It should be noted that a high pretreatment self-efficacy may indicate overconfidence and/or lack of experience with the difficulties associated with weight loss efforts 36, which is a possible limitation of the current sample of individuals. This sample of nursing-home employees were aware that they would soon be participating in a weight-loss program, which could have led to a sense of heightened self-efficacy. Individuals’ perception that the weight loss program would help make them lose weight could have swayed their perception of their own abilities, aside from the intervention they were about to undergo. However, this seems to be excessively optimistic expectations and is the norm in American obesity-treatment-seeking individuals [37].
The cross-sectional design of this analysis only captures a glimpse of the population at a specific point of time, and doesn’t capture the scope of these individuals over time. Longitudinal follow up study of the study population might have offered a better measure of factors contributing to weight change over time. The small sample size of ninety-nine individuals may also pose a limitation. Additionally, since the questionnaire was self-reported, perception of measures and response may differ from one individual to the next.
Limitations aside, findings from this analysis conclude that selfefficacy appears promising as a cognitive factor that is involved as a mediator between health behaviors and body mass index. Higher eating self-efficacy is predictive of more healthful diet, and higher exercise self-efficacy is predictive of engaging in more frequent physical activity. Higher self-efficacy involving these health behaviors may further predict a lower BMI, as is the case in the present study.
Conclusion
In conclusion, our findings further support previous research that higher self-efficacy in eating and exercise is predictive of more optimal health-related behaviors, such as healthy eating, regular exercise and lower BMI. The concept that self-efficacy as a cognitive factor can be improved upon to facilitate positive lifestyle and behavior changes is an intriguing notion in the pursuit of weight loss interventions and obesity prevention efforts. Approaches focusing on individual behavior change remains an important topic of interest in obesity research. Testing of causal mediation in the quest of behavior modification and lifestyle change is a critical step in improving future weight management interventions. This may offer the greatest possible inference for the identification of intervention variables responsible for desired health outcomes.
Human Subjects Approval
University Institutional Review Board (IRB) approval was granted for this study.
Declaration of Conflicting Interests
All Authors of this article declare they have no conflicts of interest.
Acknowledgements
This research was supported and funded by the Center for Disease Control and Prevention grant (CDC, Grant TS-1444): Principal Investigator: Dr. Pouran Faghri.
The abstract for this manuscript was accepted and presented as a poster presentation at the 26th annual Art and Science of Health Promotion Conference in Orlando, FL in April 2016.
References
- Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307: 491-497.
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, et al. (2012) Obesity and severe obesity forecasts through 2030. Am J Prev Med 42: 563-570.
- Jokinen E (2015) Obesity and cardiovascular disease. Minerva Pediatr 67: 25-32.
- Purnell JQ, Gernes R, Stein R, Sherraden MS, Knoblock-Hahn A (2014) A systematic review of financial incentives for dietary behavior change. J AcadNutr Diet 114: 1023-1035.
- Heartorg (2016) American Heart Association.
- Kim S, Popkin B (2006) Commentary: Understanding the epidemiology of overweight and obesity-a real global public health concern. Int J Epidemiol 35: 60-67.
- Stutts WC (2002) Physical activity determinants in adults. Perceived benefits, barriers and self-efficacy. AAOHN J 50: 499-507.
- Annesi JJ (2012) Supported Exercise Improves Controlled Eating and Weight through Its Effects on Psychosocial Factors: Extending a Systematic Research Program Toward Treatment Development. Perm J 16: 7-18.
- Richman RM, Loughnan GT, Droulers AM, Steinbeck KS, Caterson ID (2001) Self-efficacy in relation to eating behaviour among obese and non-obese women. Int J ObesRelatMetabDisord 25: 907.
- Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, et al. (2011) Benefits of Modest Weight Loss in Improving Cardiovascular Risk Factors in Overweight and Obese Individuals With Type 2 Diabetes. Diabetes Care 34: 1481-1486.
- Schoenborn CA, Benson V (1988) Advance Data From Vital and Health Statistics of the National Center for Health Statistics. Hyattsville, USA, 154.
- Teixeira PJ, Carraça EV, Marques MM, Rutter H, Oppert JM, et al. (2015) Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med 13: 84.
- Bandura A (1997) Self-Efficacy: The exercise of control. W. H. Freeman, New York, USA.
- Zhu D, Norman I, While A (2013) Nurses’ self-efficacy and practices relating to weight management of adult patients: A path analysis. Int J BehavNutrPhys Act 10: 131.
- Leong SL, Madden C, Gray A, Horwath C (2012) Self-determined, autonomous regulation of eating behavior is related to lower body mass index in a nationwide survey of middle-aged women. J AcadNutr Diet 112: 1337-1346.
- Wingo BC, Desmond RA, Brantley P, Appel L, Svetkey L, et al. (2013) Self-efficacy as a predictor of weight change and behavior change in the PREMIER trial. J NutrEducBehav 45: 314-321.
- Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR (1988) The development of self-efficacy scales for health related diet and exercise behaviors. Health Educ Res 3: 283-292.
- Lahiri S, Faghri P (2012) Cost-effectiveness of a workplace-based incentivized weight loss program. J Occup Environ Med 54: 371-377.
- Faghri P, Li R (2014) Effectiveness of Financial Incentives in a Worksite Diabetes Prevention Program. Open Obes J 6: 1-12.
- Bandura A (1995) Self-efficacy in changing societies. Cambridge University Press, USA.
- Kenardy J, Mensch M, Bowen K, Green B, Walton J, et al. (2001) Disordered eating behaviours in women with Type 2 diabetes mellitus. Eat Behav 2: 183-192.
- Teixeira PJ, Going SB, Sardinha LB, Lohman TG (2005) A review of psychosocial pre-treatment predictors of weight control. Obes Rev 6: 43-65.
- Raffensperger S, Kuczmarski M, Hotchkiss L, Cotugna N, Evans M, et al. (2010) Effect of race and predictors of socioeconomic status on diet quality in the HANDLS Study sample. J Natl Med Assoc 102: 923-930.
- Rehm C (2015) Socioeconomic Disparities In Health: The Role Of Diet Cost [e-book]. ProQuest Information & Learning, US.
- Rehm CD, Monsivais P, Drewnowski A (2015) Relation between diet cost and Healthy Eating Index 2010 scores among adults in the United States 2007-2010. Prev Med 73: 70-75.
- Akande VO, Hendrikss AM, Ruiter RC, Kremers SJ (2015) Determinants of dietary behavior and physical activity among Canadian Inuit: A systematic review. Int J BehavNutrPhys Act 12: 84.
- U.S. Department of Health and Human Services (2008) Physical Activity Guidelines for Americans.
- Duin D, Golbeck A, Keippel AE, Ciemins E, Fink H, et al. (2015) Using gender-based analyses to understand physical inactivity among women in Yellowstone County, Montana. Eval Program Plann 51: 45-52.
- Idowu O, Adeniyi A, Atijosan O, Ogwumike O (2013) Physical inactivity is associated with low self-efficacy and social support among patients with hypertension in Nigeria. Chronic Il 9: 156-164.
- Silva MN, Markland D, Vieira PN, Coutinho SR, Palmeira AL, et al. (2010) Helping overweight women become more active: Need support and motivational regulations for different forms of physical activity. Psychol Sport Exerc 11: 591-601.
- Silva MN, Vieira PN, Coutinho SR, Minderico CS, Matos MG, et al. (2010) Using self-determination theory to promote physical activity and weight control: A randomized controlled trial in women. J Behav Med 33: 110-122.
- Cuaderes E (2000) Predictors Of Leisure-Time Physical Activity In Adult Native American Women [e-book]. ProQuest Information & Learning, US.
- Fitzgibbon ML, Stolley MR, Kirschenbaum DS (1993) Obese people who seek treatment have different characteristics than those who do not seek treatment. Health Psychol 12: 342-345.
- Friedman MA, Brownell KD (1995) Psychological correlates of obesity: moving to the next generation. Psychol Bull 117: 3-20.
- Jakicic JM, Wing RR, Winters-Hart C (2002) Relationship of physical activity to eating behaviors and weight loss in women. Med Sci Sports Exerc 34: 1653-1659.
- Martin PD, Dutton GR, Brantley PJ (2004) Self-Efficacy as a Predictor of Weight Change in African-American Women. Obes Res 12: 646-651.
- Foster GD, Wadden TA, Wogt RA, Brwer G (1997) What is a reasonable weight loss? Patients’ expectations and evaluations of obesity treatment outcomes. J Consult ClinPsychol 65: 79-85.
Relevant Topics
- Android Obesity
- Anti Obesity Medication
- Bariatric Surgery
- Best Ways to Lose Weight
- Body Mass Index (BMI)
- Child Obesity Statistics
- Comorbidities of Obesity
- Diabetes and Obesity
- Diabetic Diet
- Diet
- Etiology of Obesity
- Exogenous Obesity
- Fat Burning Foods
- Gastric By-pass Surgery
- Genetics of Obesity
- Global Obesity Statistics
- Gynoid Obesity
- Junk Food and Childhood Obesity
- Obesity
- Obesity and Cancer
- Obesity and Nutrition
- Obesity and Sleep Apnea
- Obesity Complications
- Obesity in Pregnancy
- Obesity in United States
- Visceral Obesity
- Weight Loss
- Weight Loss Clinics
- Weight Loss Supplements
- Weight Management Programs
Recommended Journals
Article Tools
Article Usage
- Total views: 10058
- [From(publication date):
December-2016 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 8816
- PDF downloads : 1242