Research Article Open Access
Experimental Models of Microvascular Immunopathology: The Example ofCerebral Malaria
Fatima El-Assaad2, Valery Combes2 and Georges ER Grau1*
1Professor Chair of Vascular Immunology, Department of Pathology, Sydney Medical School, The University of Sydney, Address: Medical Foundation Building (K25)Room 208, 92 - 94 Parramatta Rd, Sydney, NSW, 2006, Australia
2Vascular Immunology Unit, Department of Pathology, Sydney Medical School, Medical Foundation Building, The University of Sydney Level 2, Room 20892-94 Parramatta Rd, Sydney, NSW, 2006, Australia
- *Corresponding Author:
- Georges E. R. Grau
Professor Chair of Vascular Immunology, Department of Pathology, Sydney Medical School
The University of Sydney, NSW, 2006, Australia
Medical Foundation Building (K25)Room 208, 92 - 94 Parramatta Rd
Sydney, NSW, 2006, Australia
Tel: +61 2 9036 3260
Fax: +61 2 9036 3177
E-mail: georges.grau@sydney.edu.au
Received date: April 21, 2013; Accepted date: July 14, 2013; Published date: January 06, 2014
Citation: El-Assaad F, Combes V, Grau GER (2014) Experimental Models of Microvascular Immunopathology: The Example of Cerebral Malaria. J Neuroinfect Dis 5: 134. doi: 10.4172/2314-7326.1000134
Copyright: © 2013 El-Assaad F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Human cerebral malaria is a severe and often lethal complication of Plasmodium falciparum infection. Complex host and parasite interactions should the precise mechanisms involved in the onset of this neuropathology. Adhesion of parasitised red blood cells and host cells to endothelial cells lead to profound endothelial alterations that trigger immunopathological changes, varying degrees of brain oedema and can compromise cerebral blood flow, cause cranial nerve dysfunction and hypoxia. Study of the cerebral pathology in human patients is limited to clinical and genetic field studies in endemic areas, thus cerebral malaria (CM) research relies heavily on experimental models. The availability of malaria models allows study from the inoculation of Plasmodium to the onset of disease and permit invasive experiments. Here, we discuss some aspects of our current understanding of CM, the experimental models available and some important recent findings extrapolated from these models.
Keywords
Malaria; Cerebral malaria; Experimental malaria; Plasmodium Immunopathology
Introduction
Without highly effective antimalarial treatment, death from severe Plasmodium falciparum (P. falciparum) malaria ensues just hours following admission to a hospital or clinic [1]. More than three billion individuals over a 109 malaria-endemic countries are at risk of infection, particularly children under five [2] and non-immune adults. One to two percent of individuals infected with P. falciparum develop severe malaria, with the most serious manifestation known as cerebral malaria (CM).
P. falciparum is transmitted to the human host by the female Anopheles mosquito causing a debilitating cycle of parasite differentiation, invasion and replication within the red blood cell (RBC). Rupture of the RBC and the subsequent release of parasites and their toxins activate immunological responses within the host, leading to the manifestation of this syndrome. This review addresses the value and application of data extrapolated from in vitro and in vivo models of CM to the human syndrome. We have focused on the use of human and murine microvascular endothelial cells (MVEC), retinal whole mount preparations and primate or, rodent in vivo models to discuss recently discovered parameters such as microparticles (MP) and miRNA and less on those that have been extensively reviewed previously [3-18].
Human CM: Clinical Signs and Pathophysiological Hallmarks
Immense pressure exists to quickly identify patients presenting with CM, as they are at high risk of death following hospital admission. Intensive care monitoring and antimalarial treatment is paramount to life saving care, but in resource poor countries where the highest mortality rates exist, facilities are severely limited. Those infected face poor prognosis and clinicians have a short window period in which to treat before death ensues.
The clinical presentation of CM is influenced by the immune status of the population and their level of exposure [19,20]. Notable differences in the presentation of CM exist between children and non-immune adults [21]. Typical clinical signs of P. falciparum infection include fever, nausea, malaise, anorexia, headache, joint ache and delirium [22]. Coma is the most indicative sign of CM as accessed via Blantyre coma score for children and Glasgow coma score for adults [22,23]. Other signs include seizures, respiratory distress, hypoglycaemia, circulatory collapse, spontaneous bleeding, intracranial hypertension, acidosis, prostration and severe malarial anaemia [21]. Surviving patients experience neurocognitive deficits particularly with speech and movement, post-infection [24-27].
The diagnosis of CM is based on the presence of unarousable coma, confirmation of peripheral parasitaemia and the exclusion of encephalopathies of other causes [28]. Because the diagnosis is based on exclusion, CM can be incorrectly considered in the differential diagnosis of many viral encephalopathies [29].
The pathogenesis of CM is complex, and manifestations result from interplay between several factors including those that relate to transmission parameters, virulence and drug sensitivities of P. falciparum as well those relating to the host such as genetics, nutrition and immune status.
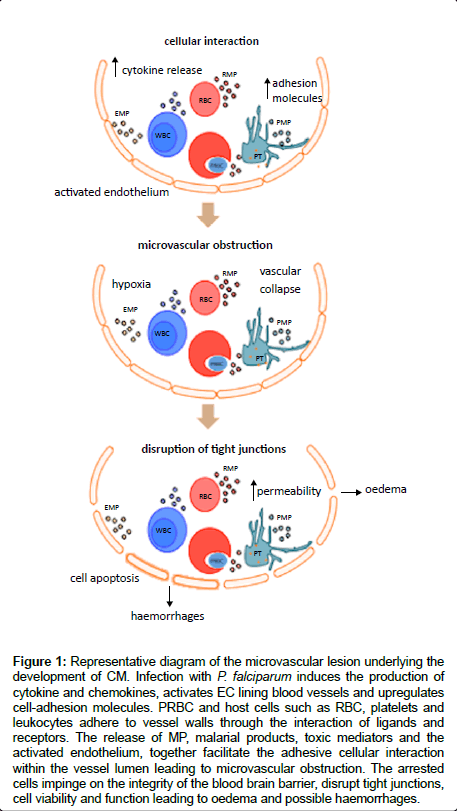
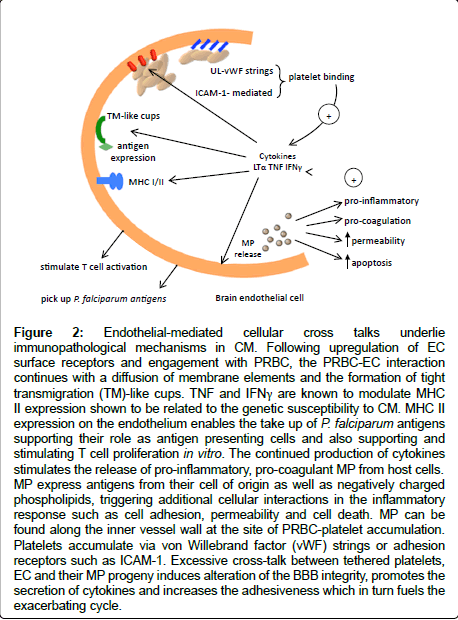
This neurovascular pathology is characterised by the sequestration of mature parasitised and non-parasitised red blood cells (PRBC and NRBC) and other cell types such as platelets and monocytes deep within the cerebral microvasculature (Figure 1) [30,31]. Ischemia due to the irreversible endothelial damage caused by the intense congestion of the vessels is believed to account for the presence of petechial and ring haemorrhages in the brain of infected patients [32]. Widespread endothelial damage by cytokines and parasite toxins result in perivascular oedema parenchymal necrosis, and neuronal cell death (Figure 2) [33,34].
Figure 1: Representative diagram of the microvascular lesion underlying the development of CM. Infection with P. falciparum induces the production of cytokine and chemokines, activates EC lining blood vessels and upregulates cell-adhesion molecules. PRBC and host cells such as RBC, platelets and leukocytes adhere to vessel walls through the interaction of ligands and receptors. The release of MP, malarial products, toxic mediators and the activated endothelium, together facilitate the adhesive cellular interaction within the vessel lumen leading to microvascular obstruction. The arrested cells impinge on the integrity of the blood brain barrier, disrupt tight junctions, cell viability and function leading to oedema and possible haemorrhages.
Figure 2: Endothelial-mediated cellular cross talks underlie immunopathological mechanisms in CM. Following upregulation of EC surface receptors and engagement with PRBC, the PRBC-EC interaction continues with a diffusion of membrane elements and the formation of tight transmigration (TM)-like cups. TNF and IFNγ are known to modulate MHC II expression shown to be related to the genetic susceptibility to CM. MHC II expression on the endothelium enables the take up of P. falciparum antigens supporting their role as antigen presenting cells and also supporting and stimulating T cell proliferation in vitro. The continued production of cytokines stimulates the release of pro-inflammatory, pro-coagulant MP from host cells. MP express antigens from their cell of origin as well as negatively charged phospholipids, triggering additional cellular interactions in the inflammatory response such as cell adhesion, permeability and cell death. MP can be found along the inner vessel wall at the site of PRBC-platelet accumulation. Platelets accumulate via von Willebrand factor (vWF) strings or adhesion receptors such as ICAM-1. Excessive cross-talk between tethered platelets, EC and their MP progeny induces alteration of the BBB integrity, promotes the secretion of cytokines and increases the adhesiveness which in turn fuels the exacerbating cycle.
Human CM: Limitations in Scope of Studies
To delineate the pathogenesis of CM, the timing and sequence of events leading to the manifestation must be known. For obvious reasons, human studies are limited to clinical and genetic field studies in endemic areas, and study of tissue at end-point, including comparative histopathology. These studies of HCM provide valuable descriptive and correlative data. Although to demonstrate causality and the underlying immunopathogenesis, invasive and interventional studies, which of course are unethical, would be required.
Current imaging technologies such as magnetic resonance imaging (MRI), spectroscopy (MRS) and computational tomography (CT) provide a way forward for clinicians to follow the progression of the disease [35,36]. Focal parenchymal abnormalities, haemorrhages or diffuse cerebral oedema attributed to CM can be detected and facilitate early diagnosis. However, these imaging technologies are expensive and their availability in endemic clinical settings is limited [22,37]. Ophthalmoscopy is less expensive alternative diagnostic tool used to detect malarial retinopathy in patients [38]. It is yet to be widely used but has great promise in increasing the precision of the clinical diagnosis of CM [38].
The limitations of human studies mandate the use of experimental models to supplement human data. Access to clinical samples is limited for ethical reasons contributing to the difficulty in validating data obtained from experimental models. Complementary methods of in vivo and in vitro experimental models as well as human studies are required to elucidate the mechanisms of pathophysiology in CM.
Models Available to Study CM
In addition to clinical field and ex vivo studies (post-mortem sampling) other approaches to studying CM include, in vitro(modelling of CM lesions) and in vivo (animal models of CM) models [39]. These model systems are empowering tools that permit the study of the sequence of events from the early stages of infection and provide a platform for the testing of novel hypotheses. They have facilitated drug testing and vaccine development as well as research on mechanisms of host defence and pathogenesis of CM [40]. Here, we have chosen to address the in vitroand in vivo experimental model contributions to our understanding of HCM, specifically regarding immunopathogenesis.
The disparity between the results extrapolated from ECM and their translation to HCM have been a matter of debate. Here we aim to address the value and application of findings observed in models of CM to the paediatric syndrome. The use of ECM is justified by the number of similarities shared with HCM [5,16]. As reviewed by Hunt and Grau in 2003, the neurological signs such as convulsions, paralysis and seizures are similar [8]. A number of key histopathological features such as vascular obstruction, parenchymal haemorrhage, leukocyte adhesion, oedema and focal demyelination are observed in ECM and in HCM [8], with PRBC accumulation substantially less marked in ECM. However, several groups have reported evidence for PRBC sequestration in ECM [41-46]. With simplified coma and behavioural scoring for ECM, similar to that routinely used to assess HCM, correlations between CM signs and cerebral changes can be made quickly [47,48].
However, the value of murine models, including the PbA model, in contributing to our current understanding of the pathogenesis of CM and therapeutic strategies has been questioned [49]. The variable incidence of PRBC sequestration, the inability of mice to be infected by P. falciparum, and the parasitological differences between human and mouse Plasmodium support this idea.
in vitro and ex vivo models
Human and mouse brain microvascular endothelial cells: in vitro models simulate the interaction between the endothelium and target cells such as RBC, platelets and MP found in the CM lesion. The endothelium of the blood brain barrier (BBB) forms the actual site of the CM lesion. Using endothelial cell lines isolated from human, mice and non-human primates, researchers have represented this interaction in both static and flow assays. MVEC have been isolated from many tissues [50], with brain and lung often used to model CM lesions, since these organs develop distinct pathology during infection. Although not a microvascular cell type, many studies have also used human umbilical cord endothelial cells in co-cultures both in static and shear-stress assays [51]. Static assays are technically simple and involve the incubation of target cells and/or parasites on subconfluent monolayers of endothelium [52]. Following incubation, non-adherent cells are washed off and adherent cells are enumerated. These static assays have contributed to our knowledge on cytoadherence although they do exclude the effect of shear forces found in blood vessels in vivo. Alternatively, flow based assays use laminar flow conditions simulating the physiological shear stress of blood vessels. These assays enable the quantitation of adherent cells, and allow close study of the receptors and ligands mediating the binding, whilst withstanding similar conditions experienced in vivo [52]. These assays can be adapted to study cytoadherence on brain, lung and placenta.
Retinal wholemount preparation: Retinopathy is an important clinical sign in adult [53,54] and paediatric CM [55]. Retinal pathology was first described in ECM [56], and can be detected by ophthalmoscopic examination of CM patients [38]. Recent studies describe damage of the optic and trigeminal nerve in ECM, explaining the manifestation of impaired visual acuity and neurological signs [57,58]. The retinal and cerebral vasculatures are so similar, that the retinal wholemount preparation provides information on the interaction of cells within an intact vascular plexus. This model allows the detection of microvascular changes such as haemorrhages, congestion and breakdown of BBB in the early stages of murine CM, including damage to the microglia and astrocytes [56,59].
in vivo models of cerebral malaria
Available animal models of CM provide a closer approximation to the human response. Although they do not reproduce HCM entirely, the key cells that are involved in the pathogenesis of HCM, experimental CM (MCM) and the immune response pathways are similar. In addition, the clinical signs and cerebral pathology, including the lesions are comparable. The most commonly used models of CM have been developed in primates and in rodents [4,39]. The number of models available to study CM pathogenesis is limited in comparison to those available to study non-severe malaria.
Primates: The importance of studying Plasmodium infection in primates has been heightened due to findings of P. falciparum in wild apes once thought as infecting humans only [60]. The cross transmission of Plasmodium between humans and primates questions host specificity and invasion strategies of the parasite. Little evidence exists to support zoonotic transmissions, although proposals into understanding the extent of the potential are underway [61,62]. Emerging evidence for P. knowlesi infection in human, potentially fatal malaria, has also supported the transfer of host from primate to human [63].
Previous attempts to produce a model that used the same causative agent as in HCM were modest. Infection of the squirrel monkey Saimiri sciureus with P. falciparum, developed neurological signs with a fatal outcome, although the model lacked predictability, with variable incidence of CM [64]. Other primate models of CM include infection of the rhesus monkey (Macaca mulatta) with P. coatneyi [65], P. knowlesi [66] or P. fragile [67], whereby infected hosts develop coma and become moribund. Post-mortem examination shows characteristic vascular congestion, notably PRBC sequestration within the brain microvessels. The overproduction of cytokines (TNF, IFN and IL-1β) and the upregulation of adhesion molecules (CD36, thrombospondin and ICAM-1) are seen in these models, mimicking pathological hallmarks of the human syndrome [68]. Although contributing to knowledge on some aspects of CM, primate model use is limited by their high cost, ethical restrictions and lack of genetically modified animals available.
Rodents: Mouse models of CM are the most commonly used in vivo experimental model [39]. Several mouse models exist in which infection is induced with Plasmodium infected RBC including P. yoelii 17XL [69], PbA [70-72] P. berghei NK65 [73] and PbK173 [74]. Each model exhibits specific characteristics, P. yoelii for instance infects preferentially reticulocytes while the others infect mature RBC. PbA mouse model has many advantages that not only include the availability of genetically susceptible and resistant mouse strains, but also the ability to reproduce clinically evident neurological signs within a precise time course. Infection of CM-susceptible mice (CBA and C57BL/6) with P. berghei ANKA (PbA) results in reproducible fatal CM, 7 to 14 days later. PbA infection of CM-resistant mice, such as the DBA/2 and BALB/c strains, results in NCM, with mice succumbing to hyperparasitaemia and severe anaemia 3 weeks later. The availability of KO strains and the relatively inexpensive breeding and housing of the mice is also an advantage. For practical and ethical reasons rodent models are commonly used to study CM.
The Contribution of Experimental Models to our Understanding of CM Pathophysiology
PRBC sequestration and cytoadherence
Sequestration of P. falciparum-infected RBC in the microvasculature, particularly small capillaries and post-capillary venules, is a signature of HCM [75-77]. P. falciparum schizonts, trophozoites as well as mature gametocytes tether and roll to adhere to host receptors. By adhering to the endothelium, RBC and parasites are removed from the circulation and consequently escape clearance by the spleen, effectively implementing their survival strategy. Analysis of post-mortem tissue from individuals who died of CM show parasite sequestration within the brain, lung, spleen, intestine, skin, fat tissue and muscle [78].
During P. falciparum infection the ability of PRBC and NRBC to squeeze through capillaries is impaired. The sequestration of the PRBC decreases the luminal diameter and the ability of erythrocytes to deform becomes very crucial to the capillary flow rate. RBC that become more rigid, plug capillary lumens already obstructed with sequestered PRBC. The growth of the parasite within the host erythrocytes modifies its shape by increasing the internal viscosity of the cell and exerts oxidative stress on the cell through release of by-products such as lactic acid. Coupled with rosetting, this obstruction leads to decreased tissue perfusion and localised hypoxia that continues the onslaught of the endothelium.
Knob proteins provide a point of attachment and have been long known to mediate parasite sequestration in P. falciparum malaria [79]. Although evidence does exist for knobless cytoadherence [80-82], suggesting other mechanisms may also contribute to this phenomenon. The absence of knobs does not necessarily diminish their ability to cytoadhere [80] validating the study of mouse PRBC, that do not display the knobbly phenotype.
The mousemodels of CM have received criticism for their inability to clearly demonstrate the sequestration phenomenon in the brain as seen in HCM. One study with P. berghei ANKA infection in (BALB/c× C57BL/6)F1mice, has clearly shown morphological evidence of PRBC and leucocyte sequestration in the brain, in a pattern similar to what is observed in HCM [41]. The accumulation of PRBC was also observed in the brain of PbA infected C57BL/6 mice [44]. Technically, detecting P. berghei sequestration in vivo is challenging. P. berghei infections are usually in asynchronous parasite stages, some stages of the cycle are indistinguishable including multiple parasite infections of a single RBC incorrectly identified as a schizont [9,43]. This hampers their detection in routine peripheral blood smears and in tissue histology. Schizonts are absent from peripheral blood smears of infected mice and only ring stages, trophozoites and gametocytes can be detected. Even technical aspects such as perfusion may also shroud the real quantitation of PRBC sequestration [44]. Also, PRBC sequestration in ECM is relatively short-lived, occurring in the final 20 hours [42], and most studies are limited by ethical constraints preventing death as the end-point.
in vitro assays using mouse brain MVEC have provided direct in vitro evidence for cytoadherence of RBC from P. berghei ANKA (PbA) and P. berghei K173 (PbK173)-infected mice on brain endothelial cells [83]. PRBC infected with P. yoelii 17XL also adhere to mouse brain MVEC [70].
From these assays the interaction of PRBC, monocytes, platelets and the CD36 receptor on MVEC [84,85] as well as the ICAM-1 [85], VCAM-1 and E-selectin receptors [86] has been described. Flow assays have confirmed the complexity of cytoadherence with a number of cell-adhesion molecules and selectins being implicated in the process of tethering, rolling and firm adhesion [87,88]. Understanding the variations in binding avidity to host ligands [89] and the pathways involved in the reversal [90] or inhibition of binding is important in finding new therapeutic strategies.
The site where the vascular endothelial cells are isolated from affects the gene expression and responsiveness to Plasmodium, thus it is important to hone in on relevant organ endothelium [77,91,92]. For example, differences exist in the mediation of cytoadherence between PRBC and the endothelium of the brain, lung and placenta. Specifically, it is known that the sequestration of PRBC in the placenta is mediated by variant surface antigens (VSA) specific for CSA, in mice and human pregnancy-related malaria [91,93]. Although, recent studies using flow cytometry-based adhesion assays, have revealed parasite adhesions other than VSA specific for CSA may also be involved [94]. Despite rodent parasites not expressing PfEMP1 homologs, mouse models of placental malaria are still informative.
The association of sequestration and clinical presentation is clear in HCM, although the causal relationship is not. Despite mouse models being criticised for not clearly demonstrating parasite sequestration, no evidence exists to suggest that the severity of HCM is related to the degree of cytoadherence [95,96].
With advancement in luciferase-based live imaging technology, evidence exists for the sequestration of PbA schizonts in the spleen, lung and adipose tissue [97], supporting the observation of organ entrapment of rodent parasites P. chabaudi chabaudi, P. vinckei petteri, P. yoelii schizonts [43,98]. The real-time in vivo imaging of these transgenic bioluminescent P. berghei parasites has enabled insight into the sequestration phenomenon in mice [97,99] as well as sporozoite interactions with host immune cells within the liver [100,101].
Parasite ligands and host endothelial receptors directly mediating sequestration of P. falciparum proteinaceous knobs on the outer membrane of RBC, erythrocyte membrane protein 1(EMP1) encoded by P. falciparum enable PRBC to bind multiple receptors such as CD36, intracellular adhesion molecule 1(ICAM-1), vascular adhesion molecule 1(VCAM-1), chondroitin sulphate A(CSA) and endothelialcell selectin (E-Selectin) [102,103]. In the mouse model, CD36 has been identified as the major receptor for schizont sequestration in lung and spleen [9,97,99]. Although no CD36 mediated schizont sequestration is observed in mouse brain, evidence exists for the close association of PRBC to the brain endothelium, closely resembling what is seen in HCM [41]. It is still unclear what mediates the sequestration of parasites in the mouse brain, although it has been shown that CD36 expressing platelets, monocytes and macrophages may facilitate the cytoadherence by serving as a bridge between the parasite and endothelium [104,105]. No clear association between the binding of CD36 and PRBC and the severity of disease exist [96,106-108]. Only sparse detection of CD36 in cerebral vessels exist, with no evidence for up regulation in human cerebral malaria [109].
Endothelial protein biomarkers such as angiopoietin-1 and 2, soluble Tie-2, von Willebrand factor (vWF), vascular endothelial growth factor (VEGF), soluble ICAM-1 (sICAM-1) are predictors of paediatric CM. More specifically, higher levels of vWF and vWF pro-peptide indicate acute endothelial cell activation in patients with malaria [110]. We now know that vWF is capable of mediating the adhesion of PRBC to the endothelium via platelet decorated ultra-large vWF strings [51]. in vitro flow assays using P. falciparum PRBC and human umbilical vein endothelial cells demonstrated this adhesionvia CD36-dependent platelet bridging and reversal was achieved by treatment with vWF proteases [51].
ICAM-1 is a major adhesion molecule on the endothelium that has been described to participate in the adhesion of PRBC to the endothelium. Upregulation of ICAM-1 expression has been observed in cerebral vessels of patients who died with CM [109]. ICAM-1- mediated sequestration of PRBC in HCM has been shown [108] and parasites isolated from children with CM showed the highest binding to ICAM-1 under flow conditions [107]. This has been confirmed on brain MVECs from patients with CM, in vitro [77]. Contact of PRBC with the endothelium mediated partially by ICAM-1, induces diffusion of malaria antigens from parasite to the endothelium and transmigrationlike cup formation, that progressively covers and engulfs the PRBC [111]. In addition to ICAM-1, PRBC form interactions with receptors CD36, P-selectin and VCAM-1 to varying degrees of strength under flow conditions [87].
Several reports of focal leucocyte recruitment in HCM [112,113] quell reports that murine models over represent the role of leucocytes in CM. Accumulation of monocytes [48,114], T cells and platelets in brain venules of PbA infected mice parallels what is observed in paediatric HCM [115] as well as adult CM [114]. Endothelial cocultures with P. falciparum demonstrate the potential for leucocyte recruitment [77,116,117].
Total parasite burden is a better indicator of disease severity. Parasite biomass accumulation within the tissue microvasculature is strongly associated with the onset of ECM [44,46] and HCM [118]. Higher parasite load is found in the brain of PbA compared to PbK173-infected mice [119]. CM-susceptible mice infected with PbK173, do not develop CM, but succumb to hyper-parasitaemia and anaemia approximately 14 days post-infection [120,121]. This parasite is used to study murine non-cerebral malaria (NCM), and resembles the pulmonary pathology seen in humans, particularly with malaria-associated ARDS [122]. The mechanism by which the parasite contributes to the pathogenesis is not straight forward. Although, it’s postulated that the parasite is responsible for the direct obstruction of microvessels following sequestration in target organs and cause anaemia through their invasion of RBC.
Cerebral oedema
Although coma in HCM is not caused by cerebral oedema [76], brain swelling and herniation still remain characteristic of CM [123,124]. In ECM, MRI studies revealed the characteristic brain oedema along with parenchymal lesions, BBB breakdown and arterial flow perturbations [125]. This oedema contributes to the compression of cerebral arteries and nerves, perturbing the blood flow and causing cranial nerve dysfunction [57]. Histologically, enlarged perivascular spaces (PVS) are signs of brain oedema that are significantly more numerous in mice with CM [126]. Interestingly, PVS are associated with an overexpression of aquaporin-4 (AQP4) on astrocytic foot processes particularly in infected mice showing signs of neurological involvement [126] but a recent study using AQP4 KO mice suggests that this molecule does not have a role in CM pathogenesis and might be protective [127]. In HCM, although not significant, a trend towards higher AQP4 was found in Vietnamese adult patients with CM [76]. This trend may be significant if studied in paediatric CM, since it resembles ECM more closely.
Hypoxia
In murine CM vascular obstruction impedes blood flow leading to ischemia, and consequently contributing to the pathogenesis of CM [128]. Intravital microscopy has revealed that ECM is associated with microvascular dysfunction, vascular collapse and decreased blood flow [129]. Interestingly, hypoxic foci are more pronounced in murine CM compared to NCM and reversal of tissue hypoxia can be achieved by injection of the hypoxia-responsive hormone, erythropoietin (EPO) [130]. EPO stimulates nitric oxide (NO) production improving tissue perfusion and oxygenation in vivo [131]. It is well established that NO in CM, modulates endothelial activation, decreases the expression of endothelial adhesion molecules and inhibits monocyte, platelet and PRBC adhesion [132-134]. Inducible synthesis of NO by the mosquito limits parasite growth [135], although direct treatment with NO does not reduce parasite growth, even at saturable levels [136]. In ECM, NO is not required for the development of the cerebral syndrome [137] and exogenous NO is protective [134]. Nitric oxide treatment reduces ICAM-1, P-selectin in the brain of PBA infected mice, and maintains the integrity of the BBB [134]. However, low bioavailability of NO contributes to the development of the syndrome in ECM [138]. In HCM, data support a deleterious role of NO [139] as well as protective [140]. Review of current data on NO has supported a hypothesis that supplemental inhaled nitric oxide (iNO) is a solid candidate for the adjunct treatment of CM [141].
Molecules and Cells Involved in CM Pathogenesis
Cytokines and chemokines
Post infection, the susceptible host undergoes a Th1 response whereby over expression of TNF, lymphotoxin (LT) and IFN exacerbates the progression to CM [142]. The overproduction of TNF and it deleterious role in CM was described in ECM and confirmed in HCM [143-145]. TNF induces alterations in the endothelium [146], mediates the upregulation of adhesion molecules, induces apoptosis [147] and the further release of cytokines and chemokines and also triggers the reorganisation of plasma membrane [148]. In human clinical trials, although patients did develop CM anti-TNF monoclonal antibody attenuated the malaria fever [149]. In C57BL/6 mice, TNF deficiency does not confer protection from CM [150] suggesting other mediators may also be contributing to the syndrome.
Since the first report of raised serum levels of LT in human CM [151], studies have shown that LT and not TNF is the principle mediator of murine CM [150]. LT deficiency in C57BL/6 mice conferred complete protection against CM [150]. Produced only by lymphocytes, LT and TNF are thought to work synergistically to induce hypoglycaemia and increased serum levels of interleukin-6 in severe malaria [151]. These overlapping functions of LT and TNF indicate that several mediators are responsible for the development of CM.
Early IFN production correlates with protection from CM and this early peak is absent in mice with CM [152]. However, late production of IFN is essential for the development of the syndrome [153]. IFN mice on CM-susceptible backgrounds are resistant to CM [154,155]. IFN influences T cell effector function and it is essential for CD4+ T cell activation, which may underlie the resistance of IFN mice to CM [156]. Incubation with IFN, increases the expression of TNF receptors [157] and the synergistic relationship between TNF and IFN has been demonstrated [158]. Recent studies have shown that neutralisation of IFNβ increased survival, reduced ICAM-1 and T-cell infiltrates in the brain [159].
Murine models of CM have allowed investigations into hostdependent mechanisms. Different mouse strains exhibit different sensitivities to Plasmodium infection and there is increasing evidence for genetic basis for susceptibility to CM [160] and the sensitivities of brain endothelium to cytokines [77,161]. PbA infection in CMsusceptible and resistant mouse strains, allow comparison in their differential responsiveness. Clinical resistance to malaria is associated with low production capacity of IFN [162]. Brain MVECs isolated from CM-resistant and sensitive mice exhibit different sensitivities to TNF [161] as did brain EC derived from patients with CM and those with uncomplicated CM [77]. Gene analysis studies of CM-susceptible and -resistant mouse strains revealed several molecular differences in early infection [163]. Variation in host gene expression may ultimately be responsible for susceptibility to infection, influencing the clinical course of malaria. Infection with PbA significantly alters the expression of genes involved in metabolic energy pathways at the time of CM [164]. This is consistent with observations of brain metabolic perturbations by way of hypoxia, hypoglycaemia and inadequate use of oxygen observed in HCM.
Platelets
in vivo and in vitro studies have supported a pathogenic role for platelets in CM [164-168]. Post-mortem sampling of brain from patients with CM showed greater accumulation of platelets and a higher proportion of vessels with platelets than brain from patients with severe malarial anaemia or non-malarial encephalopathies [169]. Close study of the CM lesion using platelet-EC assays show platelets binding to and activating the endothelium and engaging in the release and transfer of substances that may exacerbate the development of the syndrome [170]. The interaction between platelets and the endothelium dramatically modulates gene expression in vitro on human EC [171] particularly of cytokine-, chemokine-, TGFβ-, deathreceptor-, apoptosis-, erythropoietin-and TREM1-signaling pathways and potentiates cytotoxic functional changes on activated endothelium [166]. In addition, PRBC interact with CD36 expressed on platelets [172] and in synergy with TNF to induce transcriptional changes in EC [171]. Other platelet receptors gC1qR/HABP1/p32 [108] and CD31 [173] have also been identified as supporting the interaction between platelets, PRBC and endothelial cells. Imaging using a platelet-specific contrast agent revealed cytokine mediated differential platelet binding to the endothelium at earlier stages of the disease than once described using MRI [174]. As reviewed previously, platelets act as bridges between the endothelium, fibrinogen and PRBC, secreting mediators and exerting their effects at the interface of the BBB [86]. As described later in section 7, even platelet-derived microparticles enhanced P. falciparum-infected erythrocytes binding and altered EC functions similar to their parent cell [175].
T cells
Other host cells such as monocytes and T cells are active players in the pathogenesis of CM. The importance of the role of monocytes in CM pathogenesis has been reviewed previously [176]. Both CD4+ and CD8+ T cells have been implicated in HCM and ECM pathogenesis [177-179] and athymic nude mice do not develop CM [179]. Helper T lymphocytes are also involved in the pathogenesis of CM, contributing to the development of cerebral lesions with microvessel plugging and haemorrhages [70,179]. Depletion of CD4+ and CD8+ T cells reduced parasite biomass, and mice did not develop CM [44]. The concomitant presence of T cells and PRBC in the brain is critical for sequestration and the onset of CM [42,45]. CD8+ T cells accumulate in the liver in ECM, although their contribution to the progression of disease is most prominent in the brain [180]. Another line of evidence supporting this is that CD8+ T cells but no PRBC were found sequestered in the brains of mice infected with a non-CM causing parasite [42]. This was also supported in data from CM-resistant mice, where lower accumulation of PRBC and no sequestration of CD8+ T cells was observed in BALB/c mice [42]. Early evidence for leukocyte involvement in HCM [181] was later confirmed in the brains of patients who had died of CM [106,182,183].
MicroRNA
The host resistance and response to malaria is complex. Mouse models have allowed some insight into what influences susceptibility and the exploration of genes that may provide resistance to infection [11]. They have also enabled closer study of gene regulatory molecules involved in CM pathogenesis [118]. MicroRNA (miR)-150, miR-127 and let-7i, implicated in the innate immune response, apoptosis and monocytic proliferation were modulated in ECM but not in NCM [118]. Although CBA and C57BL/6 mice develop CM, they display differences in their expression of miRNA post-infection [118]. This suggests that strain differences may be a factor in gene expression regulation and this may have implications for the study of HCM, particularly with respect to differences in genetic makeup.
MP as Modulators of CM
Extracellular vesicles such as exosomes and MP have now been described as having roles in cell-cell interactions, antigen presentation and immune modulation in malarial infections [184-187]. However, so far most of studies have been made on the role MP can have as biomarkers and in the development of the disease via their interactions with target cells. Exosomes are 30–100 nm membrane vesicles derived from the endosome that carry parasite proteins and are able to elicit protective immune responses in ECM [184]. MP are larger membrane vesicles (100 nm to 1 μm) produced following cell activation and apoptosis due to cell membrane remodelling and loss of phospholipid asymmetry. During vesiculation, structural proteins are distorted, phospholipids are reorganised, and specifically through the ‘flip flop’ phenomenon phosphatidylserine (PS) migrates from the inner leaflet to the outer leaflet. The role of MP in the pathogenesis of CM has been elucidated by clinical findings and supported by in vivo and in vitro studies [185-187]. Normal baseline levels of MP are present in healthy individuals although elevated levels of circulating endothelial MP have been detected in the plasma of Malawian children with acute P. falciparum malaria [115]. Elevated levels of platelet, RBC and leucocyte-derived have been observed in patients with P. vivax malaria [188]. In Cameroonian patients, elevated levels of MP were detected from EC, monocytes, platelets and RBC in adult patients with CM [189]. Platelets released the highest levels of MP and this correlated with depth of coma and thrombocytopenia in P. falciparum-infected patients [190] and the length of acute illness and the presence of fever in P. vivax patients [188]. This finding is consistent with the presence of platelet accumulation in cerebral microvessels in HCM and ECM [105,190]. Interestingly, PMP transferred platelet antigen to PRBC and not to normal RBC and increased the PRBC cytoadherence to the endothelium [175]. Uptake of PMP by the endothelium induced changes in EC phenotypes [117,175]. Plasma concentrations of RBC derived MP were highest in patients infected with P. falciparum, compared with P. vivax and P. malariae infected and healthy patients [191]. This supports a role for MP in the exacerbation of disease.
Data collected in human studies have also been confirmed in murine CM and NCM. Interestingly, low baseline circulating MP levels were detected in non-infected mice, and subsequently raised upon CM onset [172]. Furthermore, phenotypic analyses showed that circulating MP were predominantly from platelet, endothelial and RBC origin. Mice with NCM displayed different production patterns of MP, distinct to CM mice, again supporting a role for MP in the cerebral syndrome.
TNF is an inducer of MP production in vitro [192], thus the associated elevated levels of MP during infection may be related to TNF overproduction [145]. Purified MP from mice with CM displayed significantly enhanced pro-coagulant and pro-inflammatory properties compared to healthy mice [172]. In addition these MP have adhesive properties, suggesting a potential pathogenic role in vivo [172].
Functional loss of ATP-binding cassette A-1 (ABCA-1) on the plasma membrane disables the cells ability to respond to agonists thus decreased the number of circulating MP and conferring protection against CM [172]. Prevention of CM by pantethine treatment in PbA infected mice also decreased plasma MP production [193]. Incubation with citicoline, a membrane stabiliser, prior to TNF stimulation prevents the vesiculation of MP in vitro and confers some protection in vivo when administered as adjunct therapy, in combination with artesunate [194,195].
Conclusions
Current scepticism about the relevance and use of murine models of malaria [50] has prompted a number of responses [16,40,196,197]. Some researchers voiced that this scepticism may affect grant funding and research publication that utilise experimental models [6], thus impinging on the progress of our understanding on this disease. Others called to facilitate better communication between scientists who utilise human studies and those that use experimental studies, sometimes involving the same people [6,13]. A number of recommendations have been made to improve translation of experimental data into clinical studies including the standardisation of models across all species and the creation of human tissue biobanks [13].
Appreciating the value of these models, and acknowledging their limitations would facilitate better research approaches to close the gap on CM. There are similarities between ECM and HCM to justify their use, although caution in the interpretation and application of the findings is paramount. Ultimately, the driving force for the study of HCM is the patient’s welfare and this can only be upheld by realistic translation of experimental findings.
Acknowledgements
This work was supported by grants from the National Health and Medical Research Council and the Australian Research Council.
Conflict of Interest Statement
Authors declare no competing financial interests or conflict of interests.
References
- Mishra SK, Wiese L (2009) Advances in the management of cerebral malaria in adults. Curr Opin Neurol 22: 302-307.
- Roca-Feltrer A, Carneiro I, Smith L, Schellenberg JR, Greenwood B, et al. (2010) The age patterns of severe malaria syndromes in sub-Saharan Africa across a range of transmission intensities and seasonality settings. Malar J 9: 282.
- Engwerda C, Belnoue E, Grüner AC, Rénia L (2005) Experimental models of cerebral malaria. Curr Top Microbiol Immunol 297: 103-143.
- de Souza JB, Riley EM (2002) Cerebral malaria: the contribution of studies in animal models to our understanding of immunopathogenesis. Microbes Infect 4: 291-300.
- de Souza JB, Hafalla JC, Riley EM, Couper KN (2010) Cerebral malaria: why experimental murine models are required to understand the pathogenesis of disease. Parasitology 137: 755-772.
- Langhorne J, Buffet P, Galinski M, Good M, Harty J, et al. (2011) The relevance of non-human primate and rodent malaria models for humans. Malar J 10: 23.
- Hunt NH, Golenser J, Chan-Ling T, Parekh S, Rae C, et al. (2006) Immunopathogenesis of cerebral malaria. Int J Parasitol 36: 569-582.
- Hunt NH, Grau GE (2003) Cytokines: accelerators and brakes in the pathogenesis of cerebral malaria. Trends Immunol 24: 491-499.
- Franke-Fayard B, Fonager J, Braks A, Khan SM, Janse CJ (2010) Sequestration and tissue accumulation of human malaria parasites: can we learn anything from rodent models of malaria? PLoS Pathog 6: e1001032.
- Lovegrove FE, Gharib SA, Peña-Castillo L, Patel SN, Ruzinski JT, et al. (2008) Parasite burden and CD36-mediated sequestration are determinants of acute lung injury in an experimental malaria model. PLoS Pathog 4: e1000068.
- Longley R, Smith C, Fortin A, Berghout J, McMorran B, et al. (2011) Host resistance to malaria: using mouse models to explore the host response. Mamm Genome 22: 32-42.
- Langhorne J, Quin SJ, Sanni LA (2002) Mouse models of blood-stage malaria infections: immune responses and cytokines involved in protection and pathology. Chem Immunol 80: 204-228.
- Craig AG, Grau GE, Janse C, Kazura JW, Milner D, et al. (2012) The role of animal models for research on severe malaria. PLoS Pathog 8: e1002401.
- Lamb TJ, Brown DE, Potocnik AJ, Langhorne J (2006) Insights into the immunopathogenesis of malaria using mouse models. Expert Rev Mol Med 8: 1-22.
- Sanni LA, Fonseca LF, Langhorne J (2002) Mouse models for erythrocytic-stage malaria. Methods Mol Med 72: 57-76.
- Riley EM, Couper KN, Helmby H, Hafalla JC, de Souza JB, et al. (2010) Neuropathogenesis of human and murine malaria. Trends Parasitol 26: 277-278.
- Rénia L, Potter SM, Mauduit M, Rosa DS, Kayibanda M, et al. (2006) Pathogenic T cells in cerebral malaria. Int J Parasitol 36: 547-554.
- Hansen DS (2012) Inflammatory responses associated with the induction of cerebral malaria: lessons from experimental murine models. PLoS Pathog 8: e1003045.
- Reyburn H, Mbatia R, Drakeley C, Bruce J, Carneiro I, et al. (2005) Association of transmission intensity and age with clinical manifestations and case fatality of severe Plasmodium falciparum malaria. JAMA 293: 1461-1470.
- Idro R, Aloyo J, Mayende L, Bitarakwate E, John CC, et al. (2006) Severe malaria in children in areas with low, moderate and high transmission intensity in Uganda. Trop Med Int Health 11: 115-124.
- Idro R, Jenkins NE, Newton CR (2005) Pathogenesis, clinical features, and neurological outcome of cerebral malaria. Lancet Neurol 4: 827-840.
- Taylor TE (2009) Caring for children with cerebral malaria: insights gleaned from 20 years on a research ward in Malawi. Trans R Soc Trop Med Hyg 103 Suppl 1: S6-10.
- Hanson J, Lee SJ, Mohanty S, Faiz MA, Anstey NM, et al. (2010) A simple score to predict the outcome of severe malaria in adults. Clin Infect Dis 50: 679-685.
- Boivin MJ, Bangirana P, Byarugaba J, Opoka RO, Idro R, et al. (2007) Cognitive impairment after cerebral malaria in children: a prospective study. Pediatrics 119: e360-366.
- Idro R, Ndiritu M, Ogutu B, Mithwani S, Maitland K, et al. (2007) Burden, features, and outcome of neurological involvement in acute falciparum malaria in Kenyan children. JAMA 297: 2232-2240.
- Holding PA, Stevenson J, Peshu N, Marsh K (1999) Cognitive sequelae of severe malaria with impaired consciousness. Trans R Soc Trop Med Hyg 93: 529-534.
- Dai M, Reznik SE, Spray DC, Weiss LM, Tanowitz HB, et al. (2010) Persistent cognitive and motor deficits after successful antimalarial treatment in murine cerebral malaria. Microbes Infect 12: 1198-1207.
- World Health Organization (2000) Management of severe malaria: a practical handbook. (2ndedn), Geneva: World Health Organization.
- Taylor TE, Fu WJ, Carr RA, Whitten RO, Mueller JS, et al. (2004) Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med 10: 143-145.
- Newton CR, Krishna S (1998) Severe falciparum malaria in children: current understanding of pathophysiology and supportive treatment. Pharmacol Ther 79: 1-53.
- Polder TW, Eling WM, Jerusalem CR, Wijers-Rouw M (1991) A cytochemical study of cerebrovascular lesions in mice infected with Plasmodium berghei. J Neurol Sci 101: 24-34.
- Turner G (1997) Cerebral malaria. Brain Pathol 7: 569-582.
- Grau GE, Craig AG (2012) Cerebral malaria pathogenesis: revisiting parasite and host contributions. Future Microbiol 7: 291-302.
- Schofield L, Grau GE (2005) Immunological processes in malaria pathogenesis. Nat Rev Immunol 5: 722-735.
- Patankar TF, Karnad DR, Shetty PG, Desai AP, Prasad SR (2002) Adult cerebral malaria: prognostic importance of imaging findings and correlation with postmortem findings. Radiology 224: 811-816.
- Rasalkar DD, Paunipagar BK, Sanghvi D, Sonawane BD, Loniker P (2011) Magnetic resonance imaging in cerebral malaria: a report of four cases. Br J Radiol 84: 380-385.
- Kampondeni SD, Potchen MJ, Beare NA, Seydel KB, Glover SJ, et al. (2013) MRI findings in a cohort of brain injured survivors of pediatric cerebral malaria. Am J Trop Med Hyg 88: 542-546.
- Beare NA, Taylor TE, Harding SP, Lewallen S, Molyneux ME (2006) Malarial retinopathy: a newly established diagnostic sign in severe malaria. Am J Trop Med Hyg 75: 790-797.
- Combes V, Brian De Souza J, Renia L, Hunt NH, Grau GE (2005) Cerebral malaria: Which parasite? Which model? Drug Discov Today Dis Models 2: 141-147.
- Hunt NH, Grau GE, Engwerda C, Barnum SR, van der Heyde H, et al. (2010) Murine cerebral malaria: the whole story. Trends Parasitol 26: 272-274.
- Hearn J, Rayment N, Landon DN, Katz DR, de Souza JB (2000) Immunopathology of cerebral malaria: morphological evidence of parasite sequestration in murine brain microvasculature. Infect Immun 68: 5364-5376.
- Baptista FG, Pamplona A, Pena AC, Mota MM, Pied S, et al. (2010) Accumulation of Plasmodium berghei-infected red blood cells in the brain is crucial for the development of cerebral malaria in mice. Infect Immun 78: 4033-4039.
- Franke-Fayard B, Janse CJ, Cunha-Rodrigues M, Ramesar J, Büscher P, et al. (2005) Murine malaria parasite sequestration: CD36 is the major receptor, but cerebral pathology is unlinked to sequestration. Proc Natl Acad Sci U S A 102: 11468-11473.
- Amante FH, Haque A, Stanley AC, Rivera Fde L, Randall LM, et al. (2010) Immune-mediated mechanisms of parasite tissue sequestration during experimental cerebral malaria. J Immunol 185: 3632-3642.
- Nie CQ, Bernard NJ, Norman MU, Amante FH, Lundie RJ, et al. (2009) IP-10-mediated T cell homing promotes cerebral inflammation over splenic immunity to malaria infection. PLoS Pathog 5: e1000369.
- Spaccapelo R, Janse CJ, Caterbi S, Franke-Fayard B, Bonilla JA, et al. (2010) Plasmepsin 4-deficient Plasmodium berghei are virulence attenuated and induce protective immunity against experimental malaria. Am J Pathol 176: 205-217.
- McQuillan JA, Mitchell AJ, Ho YF, Combes V, Ball HJ, et al. (2011) Coincident parasite and CD8 T cell sequestration is required for development of experimental cerebral malaria. Int J Parasitol 41: 155-163.
- Carroll RW, Wainwright MS, Kim KY, Kidambi T, Gómez ND, et al. (2010) A rapid murine coma and behavior scale for quantitative assessment of murine cerebral malaria. PLoS One 5.
- Lacerda-Queiroz N, Rodrigues DH, Vilela MC, Miranda AS, Amaral DC, et al. (2010) Inflammatory changes in the central nervous system are associated with behavioral impairment in Plasmodium berghei (strain ANKA)-infected mice. Exp Parasitol 125: 271-278.
- White NJ, Turner GD, Medana IM, Dondorp AM, Day NP (2010) The murine cerebral malaria phenomenon. Trends Parasitol 26: 11-15.
- Scott PA, Bicknell R (1993) The isolation and culture of microvascular endothelium. J Cell Sci 105 : 269-273.
- Bridges DJ, Bunn J, van Mourik JA, Grau G, Preston RJ, et al. (2010) Rapid activation of endothelial cells enables Plasmodium falciparum adhesion to platelet-decorated von Willebrand factor strings. Blood 115: 1472-1474.
- Cooke BM, Coppel RL (1995) Cytoadhesion and falciparum malaria: going with the flow. Parasitol Today 11: 282-287.
- Maude RJ, Beare NA, Abu Sayeed A, Chang CC, Charunwatthana P, et al. (2009) The spectrum of retinopathy in adults with Plasmodium falciparum malaria. Trans R Soc Trop Med Hyg 103: 665-671.
- Beare NA, Lewallen S, Taylor TE, Molyneux ME (2011) Redefining cerebral malaria by including malaria retinopathy. Future Microbiol 6: 349-355.
- White VA, Lewallen S, Beare NA, Molyneux ME, Taylor TE (2009) Retinal pathology of pediatric cerebral malaria in Malawi. PLoS One 4: e4317.
- Chang-Ling T, Neill AL, Hunt NH (1992) Early microvascular changes in murine cerebral malaria detected in retinal wholemounts. Am J Pathol 140: 1121-1130.
- Saggu R, Faille D, Grau GE, Cozzone PJ, Viola A (2011) In the eye of experimental cerebral malaria. Am J Pathol 179: 1104-1109.
- Ma N, Madigan MC, Chan-Ling T, Hunt NH (1997) Compromised blood-nerve barrier, astrogliosis, and myelin disruption in optic nerves during fatal murine cerebral malaria. Glia 19: 135-151.
- Medana IM, Hunt NH, Chaudhri G (1997) Tumor necrosis factor-alpha expression in the brain during fatal murine cerebral malaria: evidence for production by microglia and astrocytes. Am J Pathol 150: 1473-1486.
- Prugnolle F, Durand P, Neel C, Ollomo B, Ayala FJ, et al. (2010) African great apes are natural hosts of multiple related malaria species, including Plasmodium falciparum. Proc Natl Acad Sci U S A 107: 1458-1463.
- Liu W, Li Y, Learn GH, Rudicell RS, Robertson JD, et al. (2010) Origin of the human malaria parasite Plasmodium falciparum in gorillas. Nature 467: 420-425.
- Rayner JC, Liu W, Peeters M, Sharp PM, Hahn BH (2011) A plethora of Plasmodium species in wild apes: a source of human infection? Trends Parasitol 27: 222-229.
- Kantele A, Jokiranta TS (2011) Review of cases with the emerging fifth human malaria parasite, Plasmodium knowlesi. Clin Infect Dis 52: 1356-1362.
- Gysin J, Aikawa M, Tourneur N, Tegoshi T (1992) Experimental Plasmodium falciparum cerebral malaria in the squirrel monkey Saimiri sciureus. Exp Parasitol 75: 390-398.
- Nakano Y, Fujioka H, Luc KD, Rabbege JR, Todd GD, et al. (1996) A correlation of the sequestration rate of Plasmodium coatneyi-infected erythrocytes in cerebral and subcutaneous tissues of a rhesus monkey. Am J Trop Med Hyg 55: 311-314.
- Ibiwoye MO, Howard CV, Sibbons P, Hasan M, van Velzen D (1993) Cerebral malaria in the rhesus monkey (Macaca mulatta): observations on host pathology. J Comp Pathol 108: 303-310.
- Fujioka H, Millet P, Maeno Y, Nakazawa S, Ito Y, et al. (1994) A nonhuman primate model for human cerebral malaria: rhesus monkeys experimentally infected with Plasmodium fragile. Exp Parasitol 78: 371-376.
- Tongren JE, Yang C, Collins WE, Sullivan JS, Lal AA, et al. (2000) Expression of proinflammatory cytokines in four regions of the brain in Macaque mulatta (rhesus) monkeys infected with Plasmodium coatneyi. Am J Trop Med Hyg 62: 530-534.
- Kaul DK, Nagel RL, Llena JF, Shear HL (1994) Cerebral malaria in mice: demonstration of cytoadherence of infected red blood cells and microrheologic correlates. Am J Trop Med Hyg 50: 512-521.
- Grau GE, Piguet PF, Engers HD, Louis JA, Vassalli P, et al. (1986) L3T4+ T lymphocytes play a major role in the pathogenesis of murine cerebral malaria. J Immunol 137: 2348-2354.
- Bafort JM, Pryor WH, Ramsey JM (1980) Immunization of rats against malaria: a new model. J Parasitol 66: 337-338.
- Rest JR (1982) Cerebral malaria in inbred mice. I. A new model and its pathology. Trans R Soc Trop Med Hyg 76: 410-415.
- Waki S, Uehara S, Kanbe K, Ono K, Suzuki M, et al. (1992) The role of T cells in pathogenesis and protective immunity to murine malaria. Immunology 75: 646-651.
- Neill AL, Hunt NH (1992) Pathology of fatal and resolving Plasmodium berghei cerebral malaria in mice. Parasitology 105 : 165-175.
- Berendt AR, Tumer GD, Newbold CI (1994) Cerebral malaria: the sequestration hypothesis. Parasitol Today 10: 412-414.
- Grau GE, de Kossodo S (1994) Cerebral malaria: mediators, mechanical obstruction or more? Parasitol Today 10: 408-409.
- Wassmer SC, Moxon CA, Taylor T, Grau GE, Molyneux ME, et al. (2011) Vascular endothelial cells cultured from patients with cerebral or uncomplicated malaria exhibit differential reactivity to TNF. Cell Microbiol 13: 198-209.
- Seydel KB, Milner DA Jr, Kamiza SB, Molyneux ME, Taylor TE (2006) The distribution and intensity of parasite sequestration in comatose Malawian children. J Infect Dis 194: 208-205.
- Sharma YD (1997) Knob proteins in falciparum malaria. Indian J Med Res 106: 53-62.
- Ruangjirachuporn W, Afzelius BA, Paulie S, Wahlgren M, Berzins K, et al. (1991) Cytoadherence of knobby and knobless Plasmodium falciparum-infected erythrocytes. Parasitology 102 Pt 3: 325-334.
- Biggs BA, Culvenor JG, Ng JS, Kemp DJ, Brown GV (1989) Plasmodium falciparum: cytoadherence of a knobless clone. Exp Parasitol 69: 189-197.
- Udomsangpetch R, Aikawa M, Berzins K, Wahlgren M, Perlmann P (1989) Cytoadherence of knobless Plasmodium falciparum-infected erythrocytes and its inhibition by a human monoclonal antibody. Nature 338: 763-765.
- El-Assaad F, Wheway J, Mitchell AJ, Lou J, Hunt NH, et al. (2013) Cytoadherence of Plasmodium berghei-infected red blood cells to murine brain and lung microvascular endothelial cells in vitro. Infect Immun.
- Ockenhouse CF, Magowan C, Chulay JD (1989) Activation of monocytes and platelets by monoclonal antibodies or malaria-infected erythrocytes binding to the CD36 surface receptor in vitro. J Clin Invest 84: 468-475.
- Smith H, Nelson JA, Gahmberg CG, Crandall I, Sherman IW (1992) Plasmodium falciparum: cytoadherence of malaria-infected erythrocytes to human brain capillary and umbilical vein endothelial cells--a comparative study of adhesive ligands. Exp Parasitol 75: 269-280.
- Ockenhouse CF, Tegoshi T, Maeno Y, Benjamin C, Ho M, et al. (1992) Human vascular endothelial cell adhesion receptors for Plasmodium falciparum-infected erythrocytes: roles for endothelial leukocyte adhesion molecule 1 and vascular cell adhesion molecule 1. J Exp Med 176: 1183-1189.
- Udomsangpetch R, Reinhardt PH, Schollaardt T, Elliott JF, Kubes P, et al. (1997) Promiscuity of clinical Plasmodium falciparum isolates for multiple adhesion molecules under flow conditions. J Immunol 158: 4358-4364.
- Ho M, Schollaardt T, Niu X, Looareesuwan S, Patel KD, et al. (1998) Characterization of Plasmodium falciparum-infected erythrocyte and P-selectin interaction under flow conditions. Blood 91: 4803-4809.
- Adams S, Turner GD, Nash GB, Micklem K, Newbold CI, et al. (2000) Differential binding of clonal variants of Plasmodium falciparum to allelic forms of intracellular adhesion molecule 1 determined by flow adhesion assay. Infect Immun 68: 264-269.
- Jurzynski C, Gysin J, Pouvelle B (2007) CD44, a signal receptor for the inhibition of the cytoadhesion of CD36-binding Plasmodium falciparum-infected erythrocytes by CSA-binding infected erythrocytes. Microbes Infect 9: 1463-1470.
- Fried M, Duffy PE (1996) Adherence of Plasmodium falciparum to chondroitin sulfate A in the human placenta. Science 272: 1502-1504.
- Muanza K, Gay F, Behr C, Scherf A (1996) Primary culture of human lung microvessel endothelial cells: a useful in vitro model for studying Plasmodium falciparum-infected erythrocyte cytoadherence. Res Immunol 147: 149-163.
- Marinho CR, Neres R, Epiphanio S, Gonçalves LA, Catarino MB, et al. (2009) Recrudescent Plasmodium berghei from pregnant mice displays enhanced binding to the placenta and induces protection in multigravida. PLoS One 4: e5630.
- Boeuf P, Hasang W, Hanssen E, Glazier JD, Rogerson SJ (2011) Relevant assay to study the adhesion of Plasmodium falciparum-infected erythrocytes to the placental epithelium. PLoS One 6: e21126.
- Brown H, Turner G, Rogerson S, Tembo M, Mwenechanya J, et al. (1999) Cytokine expression in the brain in human cerebral malaria. J Infect Dis 180: 1742-1746.
- Rogerson SJ, Tembenu R, Dobaño C, Plitt S, Taylor TE, et al. (1999) Cytoadherence characteristics of Plasmodium falciparum-infected erythrocytes from Malawian children with severe and uncomplicated malaria. Am J Trop Med Hyg 61: 467-472.
- Smith LP, Hunter KW, Oldfield EC, Strickland GT (1982) Murine malaria: blood clearance and organ sequestration of Plasmodium yoelii-infected erythrocytes. Infect Immun 38: 162-167.
- Coquelin F, Boulard Y, Mora-Silvera E, Richard F, Chabaud AG, et al. (1999) Final stage of maturation of the erythrocytic schizonts of rodent Plasmodium in the lungs. C R Acad Sci III 322: 55-62.
- Franke-Fayard B, Waters AP, Janse CJ (2006) Real-time in vivo imaging of transgenic bioluminescent blood stages of rodent malaria parasites in mice. Nat Protoc 1: 476-485.
- Thiberge S, Blazquez S, Baldacci P, Renaud O, Shorte S, et al. (2007) in vivo imaging of malaria parasites in the murine liver. Nat Protoc 2: 1811-1818.
- Ploemen IH, Prudêncio M, Douradinha BG, Ramesar J, Fonager J, et al. (2009) Visualisation and quantitative analysis of the rodent malaria liver stage by real time imaging. PLoS One 4: e7881.
- Sherman IW, Eda S, Winograd E (2003) Cytoadherence and sequestration in Plasmodium falciparum: defining the ties that bind. Microbes Infect 5: 897-909.
- Rowe JA, Claessens A, Corrigan RA, Arman M (2009) Adhesion of Plasmodium falciparum-infected erythrocytes to human cells: molecular mechanisms and therapeutic implications. Expert Rev Mol Med 11: e16.
- Wassmer SC, Lépolard C, Traoré B, Pouvelle B, Gysin J, et al. (2004) Platelets reorient Plasmodium falciparum-infected erythrocyte cytoadhesion to activated endothelial cells. J Infect Dis 189: 180-189.
- Grau GE, Mackenzie CD, Carr RA, Redard M, Pizzolato G, et al. (2003) Platelet accumulation in brain microvessels in fatal pediatric cerebral malaria. J Infect Dis 187: 461-466.
- Aitman TJ, Cooper LD, Norsworthy PJ, Wahid FN, Gray JK, et al. (2000) Malaria susceptibility and CD36 mutation. Nature 405: 1015-1016.
- Ochola LB, Siddondo BR, Ocholla H, Nkya S, Kimani EN, et al. (2011) Specific receptor usage in Plasmodium falciparum cytoadherence is associated with disease outcome. PLoS One 6: e14741.
- Newbold C, Warn P, Black G, Berendt A, Craig A, et al. (1997) Receptor-specific adhesion and clinical disease in Plasmodium falciparum. Am J Trop Med Hyg 57: 389-398.
- Turner GD, Morrison H, Jones M, Davis TM, Looareesuwan S, et al. (1994) An immunohistochemical study of the pathology of fatal malaria. Evidence for widespread endothelial activation and a potential role for intercellular adhesion molecule-1 in cerebral sequestration. Am J Pathol 145: 1057-1069.
- Hollestelle MJ, Donkor C, Mantey EA, Chakravorty SJ, Craig A, et al. (2006) von Willebrand factor propeptide in malaria: evidence of acute endothelial cell activation. Br J Haematol 133: 562-569.
- Jambou R, Combes V, Jambou MJ, Weksler BB, Couraud PO, et al. (2010) Plasmodium falciparum adhesion on human brain microvascular endothelial cells involves transmigration-like cup formation and induces opening of intercellular junctions. PLoS Pathog 6: e1001021.
- Patnaik JK, Das BS, Mishra SK, Mohanty S, Satpathy SK, et al. (1994) Vascular clogging, mononuclear cell margination, and enhanced vascular permeability in the pathogenesis of human cerebral malaria. Am J Trop Med Hyg 51: 642-647.
- Armah H, Wired EK, Dodoo AK, Adjei AA, Tettey Y, et al. (2005) Cytokines and adhesion molecules expression in the brain in human cerebral malaria. Int J Environ Res Public Health 2: 123-131.
- Ma N, Hunt NH, Madigan MC, Chan-Ling, et al. (1996) Correlation between enhanced vascular permeability, up-regulation of cellular adhesion molecules and monocyte adhesion to the endothelium in the retina during the development of fatal murine cerebral malaria. Am J Pathol 149: 1745-62.
- Lou J, Lucas R, Grau GE (2001) Pathogenesis of cerebral malaria: recent experimental data and possible applications for humans. Clin Microbiol Rev 14: 810-820, table of contents.
- Tripathi AK, Sha W, Shulaev V, Stins MF, Sullivan DJ Jr (2009) Plasmodium falciparum-infected erythrocytes induce NF-kappaB regulated inflammatory pathways in human cerebral endothelium. Blood 114: 4243-4252.
- Faille D, El-Assaad F, Mitchell AJ, Alessi MC, Chimini G, et al. (2012) Endocytosis and intracellular processing of platelet microparticles by brain endothelial cells. J Cell Mol Med 16: 1731-1738.
- Dondorp AM, Desakorn V, Pongtavornpinyo W, Sahassananda D, Silamut K, et al. (2005) Estimation of the total parasite biomass in acute falciparum malaria from plasma PfHRP2. PLoS Med 2: e204.
- El-Assaad F, Hempel C, Combes V, Mitchell AJ, Ball HJ, et al. (2011) Differential microRNA expression in experimental cerebral and noncerebral malaria. Infect Immun 79: 2379-2384.
- Neill AL, Hunt NH (1992) Pathology of fatal and resolving Plasmodium berghei cerebral malaria in mice. Parasitology 105 : 165-175.
- Rae C, McQuillan JA, Parekh SB, Bubb WA, Weiser S, et al. (2004) Brain gene expression, metabolism, and bioenergetics: interrelationships in murine models of cerebral and noncerebral malaria. Faseb J 18: 499-510.
- Medana IM, Day NP, Sachanonta N, Mai NT, Dondorp AM, et al. (2011) Coma in fatal adult human malaria is not caused by cerebral oedema. Malar J 10: 267.
- Looareesuwan S, Wilairatana P, Krishna S, Kendall B, Vannaphan S, et al. (1995) Magnetic resonance imaging of the brain in patients with cerebral malaria. Clin Infect Dis 21: 300-309.
- Yadav P, Sharma R, Kumar S, Kumar U (2008) Magnetic resonance features of cerebral malaria. Acta Radiol 49: 566-569.
- Penet MF, Viola A, Confort-Gouny S, Le Fur Y, Duhamel G, et al. (2005) Imaging experimental cerebral malaria in vivo: significant role of ischemic brain edema. J Neurosci 25: 7352-7358.
- Ampawong S, Combes V, Hunt NH, Radford J, Chan-Ling T, et al. (2011) Quantitation of brain edema and localisation of aquaporin 4 expression in relation to susceptibility to experimental cerebral malaria. Int J Clin Exp Pathol 4: 566-574.
- Promeneur D, Lunde LK, Amiry-Moghaddam M, Agre P (2013) Protective role of brain water channel AQP4 in murine cerebral malaria. Proc Natl Acad Sci U S A 110: 1035-1040.
- Sanni LA, Rae C, Maitland A, Stocker R, Hunt NH (2001) Is ischemia involved in the pathogenesis of murine cerebral malaria? Am J Pathol 159: 1105-1112.
- Cabrales P, Zanini GM, Meays D, Frangos JA, Carvalho LJ (2010) Murine cerebral malaria is associated with a vasospasm-like microcirculatory dysfunction, and survival upon rescue treatment is markedly increased by nimodipine. Am J Pathol 176: 1306-1315.
- Hempel C, Combes V, Hunt NH, Kurtzhals JA, Grau GE (2011) CNS hypoxia is more pronounced in murine cerebral than noncerebral malaria and is reversed by erythropoietin. Am J Pathol 179: 1939-1950.
- Contaldo C, Elsherbiny A, Lindenblatt N, Plock JA, Trentz O, et al. (2009) Erythropoietin enhances oxygenation in critically perfused tissue through modulation of nitric oxide synthase. Shock 31: 599-606.
- R De Caterina, P Libby, H B Peng, V J Thannickal, T B Rajavashisth, et al. (1995) Nitric oxide decreases cytokine-induced endothelial activation. Nitric oxide selectively reduces endothelial expression of adhesion molecules and proinflammatory cytokines. J Clin Invest 96: 60-8.
- Radomski MW, Palmer RM, Moncada S (1987) Endogenous nitric oxide inhibits human platelet adhesion to vascular endothelium. Lancet 2: 1057-1058.
- Zanini GM, Cabrales P, Barkho W, Frangos JA, Carvalho LJ (2011) Exogenous nitric oxide decreases brain vascular inflammation, leakage and venular resistance during Plasmodium berghei ANKA infection in mice. J Neuroinflammation 8: 66.
- Luckhart S, Vodovotz Y, Cui L, Rosenberg R (1998) The mosquito Anopheles stephensi limits malaria parasite development with inducible synthesis of nitric oxide. Proc Natl Acad Sci U S A 95: 5700-5705.
- Rockett KA, Awburn MM, Cowden WB, Clark IA (1991) Killing of Plasmodium falciparum in vitro by nitric oxide derivatives. Infect Immun 59: 3280-3283.
- Favre N, Ryffel B, Rudin W (1999) The development of murine cerebral malaria does not require nitric oxide production. Parasitology 118 : 135-138.
- Gramaglia I, Sobolewski P, Meays D, Contreras R, Nolan JP, et al. (2006) Low nitric oxide bioavailability contributes to the genesis of experimental cerebral malaria. Nat Med 12: 1417-1422.
- Clark I, Awburn M (2002) Migration inhibitory factor in the cerebral and systemic endothelium in sepsis and malaria. Crit Care Med 30: S263-267.
- Hobbs MR, Udhayakumar V, Levesque MC, Booth J, Roberts JM, et al. (2002) A new NOS2 promoter polymorphism associated with increased nitric oxide production and protection from severe malaria in Tanzanian and Kenyan children. Lancet 360: 1468-1475.
- Hawkes M, Opoka RO, Namasopo S, Miller C, Conroy AL, et al. (2011) Nitric oxide for the adjunctive treatment of severe malaria: hypothesis and rationale. Med Hypotheses 77: 437-444.
- de Kossodo S, Grau GE (1993) Role of cytokines and adhesion molecules in malaria immunopathology. Stem Cells 11: 41-48.
- Grau GE, Fajardo LF, Piguet PF, Allet B, Lambert PH, et al. (1987) Tumor necrosis factor (cachectin) as an essential mediator in murine cerebral malaria. Science 237: 1210-1212.
- Randall LM, Engwerda CR (2010) TNF family members and malaria: old observations, new insights and future directions. Exp Parasitol 126: 326-331.
- Grau GE, Taylor TE, Molyneux ME, Wirima JJ, Vassalli P, et al. (1989) Tumor necrosis factor and disease severity in children with falciparum malaria. N Engl J Med 320: 1586-1591.
- Pober JS, Cotran RS (1990) Cytokines and endothelial cell biology. Physiol Rev 70: 427-451.
- Kimura H, Gules I, Meguro T, Zhang JH (2003) Cytotoxicity of cytokines in cerebral microvascular endothelial cell. Brain Res 990: 148-156.
- Zwaal RF, Schroit AJ (1997) Pathophysiologic implications of membrane phospholipid asymmetry in blood cells. Blood 89: 1121-1132.
- Kwiatkowski D, Molyneux ME, Stephens S, Curtis N, Klein N, et al. (1993) Anti-TNF therapy inhibits fever in cerebral malaria. Q J Med 86: 91-98.
- Engwerda CR, Mynott TL, Sawhney S, De Souza JB, Bickle QD, et al. (2002) Locally up-regulated lymphotoxin alpha, not systemic tumor necrosis factor alpha, is the principle mediator of murine cerebral malaria. J Exp Med 195: 1371-1377.
- Clark IA, Gray KM, Rockett EJ, Cowden WB, Rockett KA, et al. (1992) Increased lymphotoxin in human malarial serum, and the ability of this cytokine to increase plasma interleukin-6 and cause hypoglycaemia in mice: implications for malarial pathology. Trans R Soc Trop Med Hyg 86: 602-607.
- Mitchell AJ, Hansen AM, Hee L, Ball HJ, Potter SM, et al. (2005) Early cytokine production is associated with protection from murine cerebral malaria. Infect Immun 73: 5645-5653.
- Grau GE, Heremans H, Piguet PF, Pointaire P, Lambert PH, et al. (1989) Monoclonal antibody against interferon gamma can prevent experimental cerebral malaria and its associated overproduction of tumor necrosis factor. Proc Natl Acad Sci U S A 86: 5572-5574.
- Amani V, Vigário AM, Belnoue E, Marussig M, Fonseca L, et al. (2000) Involvement of IFN-gamma receptor-medicated signaling in pathology and anti-malarial immunity induced by Plasmodium berghei infection. Eur J Immunol 30: 1646-1655.
- Belnoue E, Potter SM, Rosa DS, Mauduit M, Grüner AC, et al. (2008) Control of pathogenic CD8+ T cell migration to the brain by IFN-gamma during experimental cerebral malaria. Parasite Immunol 30: 544-553.
- Villegas-Mendez A, de Souza JB, Murungi L, Hafalla JC, Shaw TN, et al. (2011) Heterogeneous and tissue-specific regulation of effector T cell responses by IFN-gamma during Plasmodium berghei ANKA infection. J Immunol 187: 2885-2897.
- Tsujimoto M, Yip YK, Vilcek J (1986) Interferon-gamma enhances expression of cellular receptors for tumor necrosis factor. J Immunol 136: 2441-2444.
- Pober JS, Gimbrone MA Jr, Lapierre LA, Mendrick DL, Fiers W, et al. (1986) Overlapping patterns of activation of human endothelial cells by interleukin 1, tumor necrosis factor, and immune interferon. J Immunol 137: 1893-1896.
- Morrell CN, Srivastava K, Swaim A, Lee MT, Chen J, et al. (2011) Beta interferon suppresses the development of experimental cerebral malaria. Infect Immun 79: 1750-1758.
- Waisberg M, Tarasenko T, Vickers BK, Scott BL, Willcocks LC, et al. (2011) Genetic susceptibility to systemic lupus erythematosus protects against cerebral malaria in mice. Proc Natl Acad Sci U S A 108: 1122-1127.
- Lou J, Gasche Y, Zheng L, Critico B, Monso-Hinard C, et al. (1998) Differential reactivity of brain microvascular endothelial cells to TNF reflects the genetic susceptibility to cerebral malaria. Eur J Immunol 28: 3989-4000.
- Chizzolini C, Grau GE, Geinoz A, Schrijvers D (1990) T lymphocyte interferon-gamma production induced by Plasmodium falciparum antigen is high in recently infected non-immune and low in immune subjects. Clin Exp Immunol 79: 95-99.
- Delahaye NF, Coltel N, Puthier D, Barbier M, Benech P, et al. (2007) Gene expression analysis reveals early changes in several molecular pathways in cerebral malaria-susceptible mice versus cerebral malaria-resistant mice. BMC Genomics 8: 452.
- Cox D, McConkey S (2010) The role of platelets in the pathogenesis of cerebral malaria. Cell Mol Life Sci 67: 557-568.
- Wassmer SC, Lépolard C, Traoré B, Pouvelle B, Gysin J, et al. (2004) Platelets reorient Plasmodium falciparum-infected erythrocyte cytoadhesion to activated endothelial cells. J Infect Dis 189: 180-189.
- Wassmer SC, Combes V, Candal FJ, Juhan-Vague I, Grau GE (2006) Platelets potentiate brain endothelial alterations induced by Plasmodium falciparum. Infect Immun 74: 645-653.
- Wassmer SC, Taylor T, Maclennan CA, Kanjala M, Mukaka M, et al. (2008) Platelet-induced clumping of Plasmodium falciparum-infected erythrocytes from Malawian patients with cerebral malaria-possible modulation in vivo by thrombocytopenia. J Infect Dis 197: 72-78.
- Combes V, Coltel N, Faille D, Wassmer SC, Grau GE (2006) Cerebral malaria: role of microparticles and platelets in alterations of the blood-brain barrier. Int J Parasitol 36: 541-546.
- Grau GE, Mackenzie CD, Carr RA, Redard M, Pizzolato G, et al. (2003) Platelet accumulation in brain microvessels in fatal pediatric cerebral malaria. J Infect Dis 187: 461-466.
- Faille D, El-Assaad F, Alessi MC, Fusai T, Combes V, et al. (2009) Platelet-endothelial cell interactions in cerebral malaria: the end of a cordial understanding. Thromb Haemost 102: 1093-1102.
- Barbier M, Faille D, Loriod B, Textoris J, Camus C, et al. (2011) Platelets alter gene expression profile in human brain endothelial cells in an in vitro model of cerebral malaria. PLoS One 6: e19651.
- Biswas AK, Hafiz A, Banerjee B, Kim KS, Datta K, et al. (2007) Plasmodium falciparum uses gC1qR/HABP1/p32 as a receptor to bind to vascular endothelium and for platelet-mediated clumping. PLoS Pathog 3: 1271-1280.
- Treutiger CJ, Heddini A, Fernandez V, Muller WA, Wahlgren M (1997) PECAM-1/CD31, an endothelial receptor for binding Plasmodium falciparum-infected erythrocytes. Nat Med 3: 1405-1408.
- van der Heyde HC, Nolan J, Combes V, Gramaglia I, Grau GE (2006) A unified hypothesis for the genesis of cerebral malaria: sequestration, inflammation and hemostasis leading to microcirculatory dysfunction. Trends Parasitol 22: 503-508.
- Faille D, Combes V, Mitchell AJ, Fontaine A, Juhan-Vague I, et al. (2009) Platelet microparticles: a new player in malaria parasite cytoadherence to human brain endothelium. Faseb J 23: 3449-3458.
- Hermsen C, van de Wiel T, Mommers E, Sauerwein R, Eling W (1997) Depletion of CD4+ or CD8+ T-cells prevents Plasmodium berghei induced cerebral malaria in end-stage disease. Parasitology 114 : 7-12.
- Bagot S, Nogueira F, Collette A, do Rosario V, Lemonier F, et al. (2004) Comparative study of brain CD8+ T cells induced by sporozoites and those induced by blood-stage Plasmodium berghei ANKA involved in the development of cerebral malaria. Infect Immun 72: 2817-2826.
- Coltel N, Combes V, Hunt NH, Grau GE (2004) Cerebral malaria -- a neurovascular pathology with many riddles still to be solved. Curr Neurovasc Res 1: 91-110.
- Finley RW, Mackey LJ, Lambert PH (1982) Virulent P. berghei malaria: prolonged survival and decreased cerebral pathology in cell-dependent nude mice. J Immunol 129: 2213-2218.
- Haque A, Best SE, Amante FH, Ammerdorffer A, de Labastida F, et al. (2011) High parasite burdens cause liver damage in mice following Plasmodium berghei ANKA infection independently of CD8(+) T cell-mediated immune pathology. Infect Immun 79: 1882-1888.
- Edington GM (1967) Pathology of malaria in West Africa. Br Med J 1: 715-718.
- Patnaik JK, Das BS, Mishra SK, Mohanty S, Satpathy SK, et al. (1994) Vascular clogging, mononuclear cell margination, and enhanced vascular permeability in the pathogenesis of human cerebral malaria. Am J Trop Med Hyg 51: 642-647.
- Toro G, Román G (1978) Cerebral malaria. A disseminated vasculomyelinopathy. Arch Neurol 35: 271-275.
- Martin-Jaular L, Nakayasu ES, Ferrer M, Almeida IC, Del Portillo HA (2011) Exosomes from Plasmodium yoelii-infected reticulocytes protect mice from lethal infections. PLoS One 6: e26588.
- Combes V, El-Assaad F, Faille D, Jambou R, Hunt NH, et al. (2010) Microvesiculation and cell interactions at the brain-endothelial interface in cerebral malaria pathogenesis. Prog Neurobiol 91: 140-151.
- Combes V, Coltel N, Faille D, Wassmer SC, Grau GE (2006) Cerebral malaria: role of microparticles and platelets in alterations of the blood-brain barrier. Int J Parasitol 36: 541-546.
- Combes V, Taylor TE, Juhan-Vague I, Mège JL, Mwenechanya J, et al. (2004) Circulating endothelial microparticles in malawian children with severe falciparum malaria complicated with coma. JAMA 291: 2542-2544.
- Campos FM, Franklin BS, Teixeira-Carvalho A, Filho AL, de Paula SC, et al. (2010) Augmented plasma microparticles during acute Plasmodium vivax infection. Malar J 9: 327.
- Pankoui Mfonkeu JB, Gouado I, Fotso Kuaté H, Zambou O, Amvam Zollo PH, et al. (2010) Elevated cell-specific microparticles are a biological marker for cerebral dysfunctions in human severe malaria. PLoS One 5: e13415.
- Grau GE, Tacchini-Cottier F, Vesin C, Milon G, Lou JN, et al. (1993) TNF-induced microvascular pathology: active role for platelets and importance of the LFA-1/ICAM-1 interaction. Eur Cytokine Netw 4: 415-419.
- Combes V, Coltel N, Alibert M, van Eck M, Raymond C, et al. (2005) ABCA1 gene deletion protects against cerebral malaria: potential pathogenic role of microparticles in neuropathology. Am J Pathol 166: 295-302.
- Combes V, Simon AC, Grau GE, Arnoux D, Camoin L, et al. (1999) in vitro generation of endothelial microparticles and possible prothrombotic activity in patients with lupus anticoagulant. J Clin Invest 104: 93-102.
- Penet MF, Abou-Hamdan M, Coltel N, Cornille E, Grau GE, et al. (2008) Protection against cerebral malaria by the low-molecular-weight thiol pantethine. Proc Natl Acad Sci U S A 105: 1321-1326.
- El-Assaad F (2013) Potential efficacy of citicoline as adjunct therapy in the treatment of cerebral malaria. Antimicrob Agents Chemother.
- Jambou R, El-Assaad F, Combes V, Grau GE (2009) Citicoline (CDP-choline): What role in the treatment of complications of infectious diseases. Int J Biochem Cell Biol 41: 1467-1470.
- Carvalho LJ (2010) Murine cerebral malaria: how far from human cerebral malaria? Trends Parasitol 26: 271-272.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 15072
- [From(publication date):
February-2014 - Aug 31, 2025] - Breakdown by view type
- HTML page views : 10394
- PDF downloads : 4678