Case Report Open Access
Idioventricular Rhythm in a Case of West Nile Encephalomyelitis
Ronald Espinosa1*, Kimberly Schelb2 and Antonio Liu31Department of Family Medicine, California Hospital Medical Center/University of Southern California, USA
2Ross University School of Medicine, USA
3Department of Neurology, Loma Linda School of Medicine, USA
- *Corresponding Author:
- Ronald Espinosa
Department of Family Medicine
California Hospital Medical Center/University of Southern California
Los Angeles, California, USA
Tel: 12137482411
E-mail: ronald.f.espinosa@gmail.com
Received date: April 03, 2016; Accepted date: April 29, 2016; Published date: May 02, 2016
Citation: Espinosa R, Schelb K, Liu A (2016) Idioventricular Rhythm in a Case of West Nile Encephalomyelitis. J Neuroinfect Dis 7:214. doi:10.4172/2314-7326.1000214
Copyright: © 2016 Espinosa R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Background: West nile virus (WNV), since its first appearance in the USA in 1999 has been a leading cause of viral encephalitis. There is one case report of associated fatal arrhythmia. Case: Presented is a 65 year old Hispanic male without significant past medical history presenting with West Nile Encephalomyelitis with subsequent quadriplegia and developed recurrent idioventricular rhythm requiring a permanent pacemaker. Conclusion: In the setting of West Nile Encephalomyelitis, cardiac monitoring for idioventricular rhythms and cardiac intervention should be considered.
Keywords
West nile virus; Idioventricular; Arrhythmia; Myocarditis; Encephalopathy; Pulseless electrical activity
Case Presentation
65 year old Hispanic male without known significant past medical history presents with 3 weeks of delayed mentation and body aches that began after attending an outdoor swap meet in hot weather. He developed a severe headache that resolved with acetaminophen but he became more lethargic over the next two weeks. The patient was found disoriented by family staring at himself in the mirror. Initial review of symptoms was positive for nonproductive cough, nonbloody diarrhea and nausea. During the initial hospital admission, he developed signs of meningitis and sepsis including photophobia, headache, fever and nuchal rigidity as well as acute hypoxia. Discussion with patient and family he is typically an active individual with normal exercise tolerance. The patient's medical and surgical history was negative. Family history was notable for coronary artery disease in his father and uterine cancer in his mother. There was no recent travel or known sick contacts. The initial physical exam was notable for slow responses to questions and mild bilateral lower extremity edema. Subsequent neurological exam notable for improved orientation from 2-3 with normal gait, muscle strength, and muscle sensation testing. He was placed on meningitic doses of ceftriaxone, vancomycin and acyclovir. Lumbar puncture was unsuccessful secondary to patient agitation. The Initial laboratory evaluation notable for mild transaminitis. Chest roenterogram demonstrated no acute findings.
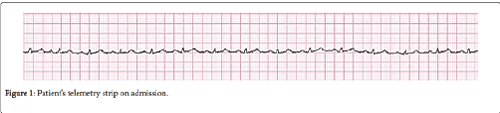
Electrocardiogram showed sinus tachycardia. He was intubated for acute respiratory failure and airway protection which was thought to be secondary to aspiration pneumonia and encephalopathy. Computed tomography angiography was negative for pulmonary embolism. The patient was stabilized and transferred to another hospital for insurance purposes two weeks later. Magnetic Resonance Imaging of the brain was performed and was negative for acute intracranial process. WNV serum titers of IgG and IgM were positive, 6.76 and 6.44 respectively. Dengue, syphilis, coccioidomycosis, cryptococcus and Guillain Barre testing were negative. He developed acute renal failure and eventually required dialysis which was likely secondary due acute tubular necrosis from ischemia from the initial hypotensive insult at the first hospital. The patient’s neurologic status worsened with development of quadriparesis shortly after transfer. His hospital course was stable until about 4 weeks after the initial presentation, when he developed idioventricular rhythm with rate approaching the 30’s, which resolved immediately upon suctioning.
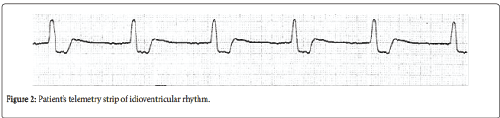
Chest roentgenogram, electrocardiogram and arterial blood gas were negative. Basic metabolic panel was essentially unchanged. One week later, the patient developed severe idioventricular episodes also to the 30’s with sinus pauses of up to 8 seconds occurring at 0317. A code blue was called for pulseless electrical activity and symptomatic bradycardia. Return of spontaneous circulation was achieved after 13 minutes with single doses atropine and epinephrine. Creatinine kinase and troponins were negative. Arterial blood gas was consistent with mild metabolic acidosis. Transthoracic echocardiogram showed hyperdynamic LV with estimated EF of 65%, and moderate RV dilation. Chest computerized tomography scanning was negative. There was no significant valvular disease. Given the severity and recurrence of his idioventricular rhythm, a permanent pacemaker was placed. No blood transfusions were given during the entirety of his hospital course. Review of the telemetry strips demonstrated few episodes of sinus tachycardia that self-resolved. The patient’s neurological status improved, initially 0/5 to 3/5 in all extremities at the time of transfer to a skilled nursing facility for rehabilitation.
Discussion
We have described a rare case where a healthy 65 year old man was found to have contracted WNV, leading to quickly improving encephalomyelitis and associated recurrent bradyarrhythmias which resultant idioventricular rhythm requiring permanent pacing. Previous studies describe encephalitis having a 1030% mortality rate and limb strength recovery taking around 68 months usually resulting in persistent weakness [1,2]. Our patient demonstrates his encephalomyelitis improving at a much faster rate than previously reported, with muscle strength testing of his distal upper extremities improving from 0/5 to 3/5 at the end of his inpatient course. Given his neurological improvement during hospitalization, his significant cardiac symptomatology necessitated more active and aggressive cardiac monitoring and intervention.
Idioventricular rhythms are defined as three or more ventricular beats with a rate less than 100, but typically fall within a range 2040 beats per minute via automaticity of the ventricular myocytes. Some common causes are myocardial ischemia, infarction, sinoatrial failure, atrioventricular failure, cardiomyopathy, hyperkalemia, medication induced and hypoxia. Review of the patient's medical record did not show significant hypoxia. No calcium channel blockers or digoxin was given, but the patient was on a stable dose of metoprolol 25 milligrams twice daily for two weeks without any episodes of bradycardia. The patient's electrolytes the day prior and after the second code blue did not show hyperkalemia. Cardiac enzymes and electrocardiograms were negative on three occasions (Table 1).
| Causes of Idioventricular Rhythm |
|---|
| Cardiac: Myocardial infarction, myocardial ischemia, sinoatrial oratrioventricular failure/block, cardiomyopathy |
| Metabolic: Hyperkalemia |
| Medication: Digoxin, nodal blocking agents |
| Respiratory: Sleep apnea, hypoxia |
| Idiopathic |
Table 1: Causes of idioventricular rhythm [10].
Since the migration of the WNV to New York in 1999 as reported by Roehrig [3], the Centers for Disease Control have documented a total of 41762 cases with 1765 deaths [4]. There have also been reports of hypercapnic respiratory failure in the setting of WNV requiring intubation [5] (Figure 1).
Myocardial involvement has been demonstrated in mammals [6]. It has been reported that cardiopulmonary manifestations were the most common complication of WNV that resulted in death [7]. Kushawaha et al. [8] describe a case report of WNV myocarditis causing a fatal arrhythmia in 2009. In a WNV outbreak in Russia in 1999, there were reported 40 postmortem cases of myocardial involvement [9,10].
Our patient experienced two episodes of bradyarrhythmias resulting in code blues during his hospital stay leading to the decision to proceed with a permanent pacemaker. With aggressive cardiac intervention, our patient was able to regain cardiac stability and be transferred to a subacute facility to continue rehabilitation for his improving quadriplegia. The implications of this case study are widespread given that WNV is now one of the most commonly reported etiologies of viral encephalitis in the United States and that there have been rare cases of fatal viral myocarditistype of arrhythmias.
Further studies are needed to determine if WNV affects not only myocardium but the sinoatrial and HisPurkinje systems (Figure 2).
A team based approach to active cardiac monitoring and aggressive intervention should be considered in cases of WNV, as well as awareness of the possible rapid improvement of WNV encephalomyelitis within the acute hospital stay.
References
- Sejvar JJ (2007) The longterm outcomes of human West Nile virus infection. Clin Infect Dis 44: 1617–1624.
- Sejvar JJ (2014) Clinical Manifestations and Outcomes of West Nile Virus Infection. Viruses 6: 606623.
- Roehrig J (2013) West Nile Virus in the United States A Historical Perspective. Viruses 5: 30883108.
- http://www.cdc.gov/westnile/resources/pdfs/data/1wnvdiseasecasesbyyear 19992014_06042015.pdf
- Tso G, Kaldas K, Springer J, Barot N, Kamangar N (2015) West Nile Meningoencephalitis Presenting as Isolated Bulbar Palsy with Hypercapnic Respiratory Failure: A Case Report and Literature Review. Journal of Intensive Care Medicine 13.
- van der Meulen KM, Pensaert MB, Nauwynck HJ (2005) West Nile virus in the vertebrate world. Arch Virol 150: 637657.
- Sevjar J, Lindsey N, Campbell GL (2011) Primary Causes of Death in Reported cases of Fatal West Nile Fever, United States 20022006. VectorBorne and Zoonotic Diseases 11: 161164.
- Kushawaha A, Jadonath S, Mobarakai N (2009) West Nile Virus Myocarditis Causing a Fatal Arrhythmia: A case report. Case Journal 2: 7147.
- Platonov AE, Shipulin GA, Shipulina OY, Tyutyunnik EN, Frolochkina TI, et al. (2001) Outbreak of West Nile Virus infection, Volgograd Region, Russia, 1999. Emerg Infect Dis 7: 128132.
- http://accessmedicine.mhmedical.com/content.aspx?bookid=1130&Sectionid=7974 2328.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 12217
- [From(publication date):
June-2016 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 11216
- PDF downloads : 1001