Research Article Open Access
Meningitis Outbreaks due to Neisseria meningitidis in 2010 and 2012 in Burkina Faso
Savadogo M1*, Yelbeogo D2, Zabsonre S3, Tarbagdo F2, Koussoube D2 and Ouedraogo A4
1CHU YO Infectious Diseases Department, Burkina Faso
2Directorate for fighting Diseases, Burkina Faso
3CHU YO Neurosurgery Department, Burkina Faso
4CHU YO Psychiatry Department, Burkina Faso
- *Corresponding Author:
- Mamoudou S
Department of Infectious Diseases
Yalgado Ouedraogo Hospital, Burkina Faso
Tel: +70259154
E-mail: savadoma@gmail.com
Received January 18, 2015; Accepted March 27, 2015; Published March 29, 2015
Citation: Savadogo M, Yelbéogo D, Zabsonré S, Tarbagdo F, Koussoubé D, et al. (2015) Meningitis Outbreaks due to Neisseria meningitidis in 2010 and 2012 in Burkina Faso. J Neuroinfect Dis 6:171. doi: 10.4172/2314-7326.1000171
Copyright: ©2015 Mamoudou S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
During the epidemic seasons in 2010 and 2012, epidemic outbreaks were recorded in several health districts in Burkina Faso. Objective: Describing the epidemiology characteristics and response during epidemics of 2010 and 2012. Patients and methods: It consisted in a descriptive cross-sectional study which was conducted during epidemics of 2010 and 2012. Data were collected in health districts. Meningitis cases are defined as suspect, probable or confirmed cases according to WHO definitions. The data were entered and analyzed using Epi Info 3 5 1. Outcomes: Twelve districts had crossed their epidemic threshold in 2010 and thirteen in 2012. The isolated bacteria were dominated by Neisseria meningitidisX in 2010 and Neisseria meningitidis W in 2012. The average age of patients was 12 years in 2010 and 9 years in 2012. The sex ratio was 1.3 in 2010 and 1.3 in 2012 in favor of the male. The modal age group was that of 5 and 14 years respectively in 2010 and 2012. Three health districts had a vaccine response with uncombined polysaccharide vaccine ACYW. The appropriate management of cases and children immunity strengthening remain major strategies against meningitis epidemics. It is important to acquire combined tetravalent ACYW vaccine for adapted vaccine response in case of epidemics.
Keywords
Meningitis; Epidemics; Neisseria meningitides; Burkina Faso
Introduction
Burkina Faso is located in the middle of West Africa, within the band expanding from the Red Sea to the Atlantic, described in 1963 by Lapeyssonnie as the African meningitis belt. In this area are regularly recorded epidemic outbreaks occurring periodically. In Burkina Faso these epidemics are a real public health issue [1]. Climatic conditions, poverty and poor population immunity make it possible for the emergence of recurrent meningitis outbreaks by Neisseria meningitidis. Neisseria meningitidis of serogroup A was formerly responsible for most outbreaks [2-4], but vaccination of the population in 2010, with the new combined antimeningococcal A vaccine (MenAfriVac) significantly reduced this form of meningitis in favor of other serogroups of Neisseria meningitidis. We describe the characteristics of the outbreaks which took place in 2010 and 2012 in Burkina Faso.
Patients and Methods
Data were collected at health districts. Meningitis cases are defined as suspect, probable or confirmed cases (9) corresponding to the inclusion criteria. Weekly attack rates are obtained by the ratio of the number of cases on the district population, and are expressed in number of cases per 100,000 inhabitants. They allow the definition of epidemic thresholds at district level. Thus, a district is on alert when it shows 5-9 cases per 100 000 inhabitants in a week and in epidemics when it showed at least 10 cases per 100 000 inhabitants in a week. Data were entered and analyzed using Epi Info 3 5 1.
Outcomes
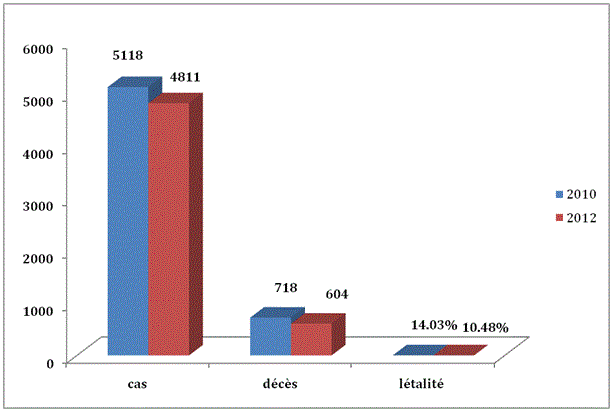
Epidemiological aspects: 12 health districts crossed their epidemic threshold in 2010 and 13 in 2012. The average age was 12 years and 9 years respectively in 2010 and 2012. The sex ratio was 1.3 in 2010; and 1.3 in 2012 in favor of men. The modal age group was that of 5 to 14 years. Figure 1 shows the cases, deaths and lethality due to meningitis in 2010 and 2012.
Figure 1: Distribution of cases and deaths in 2010 and in 2012.Neisseria meningitidis X was the dominant organism in 2010. This organism was responsible for epidemiologic outbreaks in 12 health districts out of 63. In 2012, it was Neisseria meningitidis W that was responsible for epidemiologic outbreaks in 13 out of the 63 health districts.
Response to epidemics
Three health districts benefited from a reactive vaccination campaign with the uncombined polysaccaridique vaccine (A, C, Y, W) in 2012. In the absence of vaccine against serogroup X, health officials had suppliedthe health districts withspecific drugs (ceftriaxone and ampicillin, according to national guidelines) allowing free treatment of meningitis cases. Deficiencies in the management were noted such as late diagnosis, a non-compliance with treatment protocols by health workers, deficiency in managing treatment drugs and late consultations of patients.
Discussion
Neisseria meningitidis X was for the first time responsible for meningitis epidemics in Burkina Faso in 2010, with 14.03% lethality. In the absence of vaccine against serogroup X, the main strategy used by health authorities was the free treatment of cases and awareness raising for early use of health structures. In 2012, it is Neisseria meningitidis W that was responsible for several outbreaks in 13 districts, with lethality of 10.4%. This lethality has not varied much over the years since it was 11.5% in 1992 and 2002 [5]. All epidemics due to Neisseria meningitides W had the same difficulty, that was the one related to lack of vaccine containing the W valence for rapid and adapted immunization response as recommended by WHO. As Bertherat [6], we find that the occurrence of outbreaks by N. meningitides W, is a challenge in terms of epidemic response due to the poor production capacity of the tetravalent vaccine [6]. In addition, the unconjugated polysaccaridique vaccine (including the quadrivalent A, C, Y, W) does not offer an extended individual immunity. The short duration of immunity makes it possible to limit the spread of the epidemic for one or two transmission seasons, but no more [7]. Moreover, unlike the combined vaccine that controls nasopharyngeal carry [8], the polysaccharide vaccine induces low group immunity, reducing its impact on the spread of the epidemic. The high cost of tetravalent vaccine (A, C, Y, W) and supply problems make it necessary to strengthen the monitoring and improving the management of meningitis cases in high-risk countries such as Burkina Faso [6]. Vigilance will be particularly in districts that have not undergone recent outbreak by N. meningitidis W because the population is less immunized there and therefore is more exposed [8,9].
Conclusion
The emergence of N. meningitidis W and N. meningitidis X changed the epidemiological situation of meningitis in Burkina Faso. There remains a risk of occurrence of these outbreaks due to the absence of a vaccine against N. meningitidis X and allow immunization coverage against N. meningitides W. It is important to build the capacity of laboratories and health care facilities for appropriate case treatment.
References
- Zombré S, Hacen MM, Ouango G, Sanou S, Adamou Y, et al. (2007) The outbreak of meningitis due to Neisseria meningitidis W135 in 2003 in Burkina Faso and the national response: Main lessons learn. Vaccine 25: 69-71.
- Nicolas P (2012) Épidémies de méningite à méningocoquesdans la ceinture de la méningite (1995-2011) et introduction du vaccinméningococcique A conjuguéMédecineetSante´ Tropicales 22: 246-258.
- Lapeyssonnie L (1963) La meningitecérébrale en afrique OMS Génève.
- Koumaré B, Ouedraogo-Traoré R, Sanou I, YadaAA, Sow I (2002) The first large epidemic of meningococcal disease caused by serogroup W135, Burkina Faso.Vaccine 25: 37-41.
- Bertherat E, Yada A, Djingarey MH, Koumare B (2002) en collaboration avec le ministere de la sante et la representation oms au burkinafasoPremièreépidémie de grandeampleurprovoquée Par Neisseria meningitidis w 135 en Afrique.Med Trop 62: 301-304.
- SanouI,Ouedraogo-Traoré R, Ki- zerbo GA, Bicaba I, Kam L, et al. (2006) Méningites à méningocoque du sérogroupe w135: Étude de 148 casobservés en 2002 et en 2003 au CHU YO de Ouagadougou, Burkina Faso.Med Trop66: 137-142.
- WHO.Luttecontre les épidémies de méningite à méningocoque:Guide pratique OMSWHO/EMC/BAC/98.3.
- Alonso JM, Bertherat E, Perea W, Borrow R, Chanteau S, et al.(2006) Sow Ceintureafricaine de la méningite : de la génomique aux stratégies de surveillance, de lutte et de prévention (colloqueorganiséparl’Institut Pasteur et le CERMES, avec le soutien de la FondationMérieux – Niamey, Niger, 26-29 novembre 2005)Bull SocPatholExot 99: 404-408.
- OMS (2000) Détecteruneépidémie de méningite à méningocoquedans les pays à forte endé micité en Afrique. WklyEpidemiol Rec 75:306-309.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 14103
- [From(publication date):
May-2015 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 9566
- PDF downloads : 4537