Research Article Open Access
Needs for Palliative Care of Cancer Patients in Brazil: Analysis of Data from 2008-2014
Cledy Eliana dos Santos1*, José Manuel Peixoto Caldas2, José Américo Serafim3, Newton Barros4, Altamiro da Costa Pereira5, Marcelo Eduardo Zanella Capra6 and Airton Stein7
1Community Health Service and Palliative Care Service, Hospital Nossa Senhora da Conceição - GHC (Grupo Hospitalar Conceição), Brazil
2Department of Education and Medical Simulation, University of Porto-Portugal; Visiting Professor of Post-Graduate Program in Collective Health from UNIFOR, Brazil
3Information Technology Department of the Brazilian Health System-SUS (DATASUS), Ministry of Health, Brazil
4Palliative Care Service, Hospital Nossa Senhora da Conceição-GHC (Grupo Hospitalar Conceição)
5Director of the CINTESIS - FMUP, Brazil
6Oncology Service, Hospital Nossa Senhora da Conceição-GHC (Grupo Hospitalar Conceição), Brazil
7Community Health Service and Teaching and Research Management, Hospital Nossa Senhora da Conceição-GHC (Grupo Hospitalar Conceição), Brazil
- *Corresponding Author:
- Eliana dos Santos C
Community Health Service and Palliative Care Service
Hospital Nossa Senhora da Conceição - GHC (Grupo Hospitalar Conceição), Brazil
Tel: +5551 3357 2140
Fax: +5551 32551744
E-mail: cledy.eliana@gmail.com
Received date: November 15, 2016; Accepted date: December 21, 2016; Published date: December 26, 2016
Citation: dos Santos CE, Peixoto Caldas JM, Serafim JA, Barros N, da Costa Pereira A, et al. (2017) Needs for Palliative Care of Cancer Patients in Brazil: Analysis of Data from 2008-2014. J Palliat Care Med 7:294. doi: 10.4172/2165-7386.1000294
Copyright: © 2017 dos Santos CE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: The Brazilian Health System (SUS) faces major challenges to ensure the constitutional right of universal access to health care assistance and technological advances to the entire population. Concerns with the ageing population, the increasing incidence of cancer and the emergence of chronic non-communicable diseases include palliative care as one of the objectives of the Brazilian Health System (SUS). However, considering that each disease and individual present different social and cultural factors, needs, pattern of disease progression, associated co-morbidities and access to health care, the estimation of necessary resources and the definition of specific criteria to structure and adapt palliative care in the health services have been a difficult task in Brazil. Thus, it is necessary to estimate the needs and the resources and to specify parameters to structure and tailor an adequate modality of assistance in palliative care. Aims: 1) To estimate the number of cancer patients with palliative care needs in the population; 2) To simulate palliative care methods for population based estimation. Methods: The present methodology has a quantitative approach, with descriptive, exploratory, retrospective and observational studies of hospitalized cancer patients. This is a cross-sectional study using death certificate and hospital admission data, which was collected from the Mortality Information System (SIM) and Hospital Information System (SIH) of the Brazilian Health System (SUS), obtained from the database of the Health Information Department (DATASUS). Results: Yearly around 1.1 million deaths were reported to the Brazilian Mortality Information System, being 15.9% of these related to people living with cancer. Between 2008 and 2014, there were almost 4.5 million hospitalizations (4,431,685) of patients with cancer in Brazil, and, of all the hospital admissions of cancer patients, 1.189.908 (26.85%) were related to intercurrences of the disease and/or of treatment. The average rate of hospital mortality was 7.7 for cancer in general and 21.4 for clinical intercurrence of cancer patients, while the average length of stay (LOS) was 5.7 days for cancer in general and 7.9 days for clinical intercurrence of cancer patients. Conclusion: considering that the offer and the technical guidance regarding palliative care for users served by health establishments authorized by Brazilian Health System for the specialized assistance in oncology are mandatory, we need to estimate the needs, resources and specify parameters to structure and tailor an adequate modality of assistance in palliative care.
Keywords
Cancer; Palliative care needs; Estimate cancer palliative care population; Clinical intercurrences in oncological patients; Hospital admissions of cancer patients
Introduction
Systematic analysis on the subject shows that the disease prevention and curative treatments have been the main goals of the health professionals, being the incurability processes and often reputed death considered as failure. When the character of the cure has to be immediate, the implementation of actions directed to the comprehensive care of people with advanced chronic diseases or in the final stages of life, as well as the necessary help to maintain or achieve a life with dignity and quality, has been a challenge. Besides, when the model of curative medicine is focused essentially on the disease, this model does not meet all the needs of people living with chronic advanced diseases or people who do not respond to curative treatment. According to the World Health Organization (WHO), each year more than 40 million people require palliative care and 20 million people need palliative care at the end of life worldwide [1,2].
The Pan American Health Organization (PAHO) designs, for the year of 2020, the occurrence of 840.000 cancer deaths in Latin America and the Caribbean, and call attention to the fact that palliative care has not been valued in people with cancer, when they should be part of the treatment from the time of diagnosis [3].
However, the World Health Organization (WHO) demonstrates that approximately 80% of cancer patients need terminal palliative care and at least 80% of persons who died as a result of cancer and other life-threatening diseases could benefit from palliative care [4,5]. To the year 2030, 27 million new cases of cancer, 17 million deaths (caused by cancer) and 75 million people living with the disease are expected worldwide. The biggest effect of this increase will focus on low-and middle-income countries [6]. Brazil currently has a population of approximately 206 million people, with a large regional diversity and a variety of ethnicities - 47.7% of whites, 43.1% of mulattos (mixture of whites and blacks), 7.6% of blacks, 1.1% of Asians and 0.4% of indigenous - distributed in a wide territory [7].
The demographic and epidemiologic transition in the country has been deeply marked by low fertility rates, fast ageing and increasing life expectancy resulting in rise of chronic non-communicable diseases. This process of demographic transition, called “ageing population”, associated with the transformation in the relationship between people and their environment, brought a major change in the profile of morbidity and mortality, decreasing the occurrence of infectious diseases and laying the chronic non-communicable diseases as the new center of attention in the problems of disease and death of the Brazilian population. Nevertheless, the setting of cancer trends rates and burden, associated with longer chronic disease trajectories and greater co-morbidity, is producing a major impact on public health policy, requiring further incentives to improve and expand palliative care provision. The distribution of different types of cancer in Brazil suggests an epidemiological transition in progress [8-11].
With recent fast ageing population, which designs the exponential growth of the elderly, it is possible to identify a significant increase in the prevalence of cancer, requiring immense effort for the provision of adequate attention to patients. In this context, the Brazilian Health System faces major challenges to ensure the constitutional right of universal access to health care assistance and technological advances to the intire population. Concerns with the ageing population, the increasing incidence of cancer and the emergence of chronic noncommunicable diseases include palliative care as one of the objectives of the Brazilian Health System [12,13].
Cancer is a disease that can appear silently, being so often diagnosed at an advanced stage hindering treatment success and decreasing the chances of cure [14]. The Brazilian National Policy for Cancer Prevention and Control ensures integral assistance to any person with cancer, by means of High Complexity Assistance Unit in Oncology (Unacon) and High Complexity Assistance Center in Oncology (Cacon) [15]. In Brazil, about 60% of cancer patients are diagnosed at an advanced stage. In the case of lung cancer, 87.9% of the cases are discovered late [16-19]. Therefore, it becomes imperative to improve the quality of care, to facilitate the access to palliative care and to promote equity in health services [20,21]. Considering that each disease and individual present a different pattern of disease progression and a variety of factors including age, co-morbidities and level of care, the estimation of necessary resources and the definition of specific criteria to structure and adapt palliative care have been a big challenge to the Brazilian health care system [22-30].
So far, we have used as reference the experiences of countries which have a well-structured assistance policy and established parameters for estimation of health care resources at different levels of attention.
However, it is important to analyze the applicability of these models in the reality of our country, as well as to sensitize health professionals for a full and humanized understanding regarding the complexity of attention that a patient with serious or advanced illness in the final stage of life, including their families, demands.
The main goals of this study were to analyse cancer patients who could benefit from palliative care in Brazil, through the outline of national death certificate and hospital admission of cancer patients in the Brazilian Health System (SUS) for treatment of clinical intercurrences related to cancer, and to estimate the target population with palliative care needs between 2008 and 2014. An ecological and historical series study was performed using national secondary data from mortality information system and hospital admissions related to cancer. In addition, the specific goals for this research are: to analyze the demand of patients for palliative care and to verify the use of hospital beds for admission of patients with oncologic clinic intercurrences.
Health policy
The 1988 Brazilian Federal Constitution recognized health as a citizen’s right and a duty of the state, and established the basis for the creation of SUS, which was based on the principles of universality, integrity, and social participation [31]. Brazilian health-policy has been considering, for several decades, the universal access to health care, social reintegration, the need to enhance the hospital care for chronic patients suffering from multiple problems, convalescence and/or in need of permanent care requiring continuous assistance and physical and functional rehabilitation. The Brazilian Health System (SUS) is one of the largest public health systems in the world. Formed by a complex network of public and private institutions dedicated to providing, financing, and managing health services. Presently, three-quarters of the Brazil’s 206 million inhabitants depend on free care from SUS [32,33]. In the last decades, several initiatives by the Brazilian Ministry of Health have incorporated palliative care as an important strategy for the health policy [34-43].
According to the Brazilian National Oncological Care (Decree GM/MS 2.439/2005), cancer control, like other chronic diseases, must contain all actions and health services available in the Brazilian Health System (SUS): health promotion, prevention, diagnosis, treatment, rehabilitation and palliative care [44]. With the goal of improving the quality of life, relieving physical suffering, catering for the psychological, spiritual and social needs of people with serious and advanced diseases and providing support to families and caregivers, it becomes necessary to promote reflection on the existing models of care, to meet the size, nature and severity of the needs of people with regard to palliative care and to motivate the inclusion or expansion of this type of care in the practice of comprehensive health care, following the principles of SUS: Universality, Equity and Completeness of health care [44].
Chronic diseases
Brazilian health-policy has been considering, for several decades, the need to enhance the chronic patients suffering from multiple harms to health, convalescents and/or permanent care requiring continues care, physical and functional rehabilitation, with a view to social reintegration. Database records of Mortality Information System of the Brazilian Health System (SIM - DATASUS) show that, since 2003, the general mortality in Brazil comes surpassing 1 million people per year.
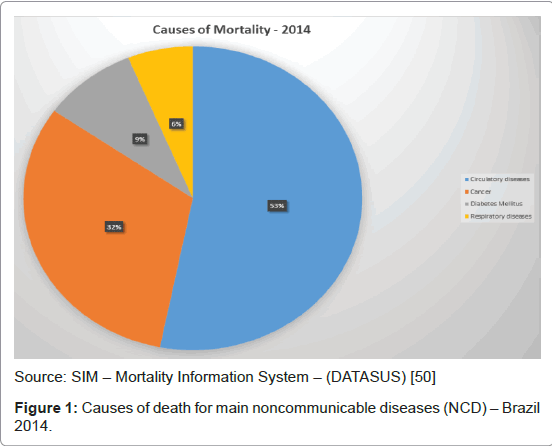
According to the Brazilian Mortality System, 1,227,039 deaths were registered in 2014, being the death rate up to 6038.58 per million of inhabitants, per year. In Brazil, approximately 74% of deaths registered, in the period between 2008 and 2014, were related to chronic non communicable diseases (NCD). This sets up a change in the burden of diseases and presents a new challenge for managers of health. The stronger the impact of NCD in the quality of life of affected individuals, the greater the chance of premature death and the adverse economic effects for families, communities and society in general [45]. The four most prevalent chronic diseases highlighted by WHO [46] accounted for 52% of deaths in the years of 2008 and 2014 in Brazil. Concerning the average distribuition of diseases in both years, cardiovascular diseases account for most NCD deaths (54%), followed by cancer (31%), diabetes (9%) and respiratory diseases (6%) (Table 1). Within the framework of chronic diseases, cancer deserves a differentiated approach, for its high prevalence, consumption of large amounts of financial resources, and its big institutional and social burden [47-49] (Figure 1).
| Main NCD | Number of deaths | Percentage (%) of diseases deaths/Total NCD deaths | |||
| 2008 | 2014 | Variation 2008/2014 | 2008 | 2014 | |
| Diabetes Mellitus | 50.448 | 57.288 | 14 | 9 | 9 |
| Circulatory diseases | 317.797 | 337.611 | 6 | 56 | 53 |
| Respiratory diseases | 34.913 | 39.642 | 14 | 6 | 6 |
| Cancer | 167.677 | 200.979 | 20 | 29 | 32 |
| Total of deaths/ main NCD | 570.835 | 635.52 | 11 | 100 | 100 |
| Total deaths/year | 1,077.01 | 1.222.381 | 13 | - | - |
| % NCD deaths | 53 | 52 | 52 | - | - |
Table 1: Leading causes of death for main noncommunicable diseases (NCD) in Brazil.
Cancer in Brazil
Cancer figures among the leading causes of morbidity and mortality in Brazil, with approximately 576.000 new cases and around 202.000 cancer related deaths in 2014. According to the Brazilian National Oncology Policy, cancer control must include health promotion, rehabilitation, and palliative care, following the Brazilian Health System (SUS) principles: Universality, Equity and Completeness of health care. The incidence ofcancer grows in Brazil, as all over the world, at a rate accompanying the ageing population, resulted from the increase of life expectancy. This is a direct result of the great global transformations of recent decades, which has changed the situation of people’s health by the accelerated urbanization, new lifestyles and new patterns of consumption [47-49].
The total incidence of cancer in Brazil grew by 70% in the period from 2001 to 2014 and 11% in the period from 2008 to 2014. Estimates for 2014, valid also for 2015, point to the occurrence of approximately 576.580 new cases of cancer, including cases of non-melanoma skin cancer, reinforcing the magnitude of the problem of cancer in the country. In the same years, a total of 302,350 new cases of cancer for males and 274,230 for females are expected. The cancer type non-melanoma skin (182,130) will have the highest incidence in the Brazilian population, followed by prostate tumors (69.000), female breast (57,000), colon and rectum (33,000), lung (27,000), stomach (20,000) and cervix (15,000) [49,51].
By excluding the cases of non-melanoma skin cancer, there was an estimated total of 395 thousand (68.5%) new cases of malignant tumours [51], being the gender distribution 204,000 for males and 191,000 for females. In men, the most incident kinds of cancers are the prostate, lung, colon and rectum, stomach and oral cavity; and, in women, the breast, colon and rectum, cervix, lungs and thyroid gland [13].
Cancer mortality
Yearly an average of 1.1 million deaths, considering all causes, are reported to the Brazilian Mortality Information System (SIM), being 15.9% related to people living with cancer. Cancer mortality increased by 17.5% between 2008 and 2014 and, since 2003, cancer represents the second cause of death by disease group in the Brazilian population.
While the General mortality in Brazil had an increase of 27.1%, and the population grew 15.3%, cancer mortality had an increase of 60.3% in the period between 2001 (125.348) and 2014 (200.979). Thus, the gross rate of cancer mortality had an increase of 39% between 2001 (0.71/1,000 inhabitants) and 2014 (0.99/1,000 inhabitants).
According to the Mortality Information System of the Brazilian Health System (SIM - SUS), 201,968 cancer deaths were register throughout the country in 2014. In the same year, 725,685 patients with cancer were admitted at SUS hospitals network. Out of these hospitalizations, 57,697 (8.0%) resulted in death (Table 2 and Figure 2).
| Year | Cancer mortality - Mortality Information System | ||||||
| Total mortality | Total of cancer deaths | Percentage (%)of total cancer death | Male cancer death | Percentage (%)of male cancer death | Female cancer death | Percentage (%)of female cancer death | |
| 2008 | 1,077.01 | 167.677 | 15.60 | 90.176 | 53.80 | 77.49 | 46.20 |
| 2009 | 1.103.088 | 172.255 | 15.60 | 92.515 | 53.70 | 79.732 | 46.30 |
| 2010 | 1.136.947 | 178.99 | 15.70 | 96.168 | 53.70 | 82.792 | 46.30 |
| 2011 | 1.170.498 | 184.384 | 15.80 | 98.444 | 53.40 | 85.931 | 46.60 |
| 2012 | 1.181.166 | 191.577 | 16.20 | 101.974 | 53.20 | 89.596 | 46.80 |
| 2013 | 1.210.474 | 196.954 | 16.30 | 105.211 | 53.40 | 91.723 | 46.60 |
| 2014 | 1.222.381 | 201.968 | 16.50 | 107.306 | 53.10 | 94.631 | 46.90 |
| Total | 7.024.554 | 1.293.805 | 15.90 | 691.794 | 53.50 | 601.895 | 46.50 |
Table 2: Cancer mortality (2008-2014).
Clinical intercurrences in oncological patients
In recent years, in Brazil, we have seen an increased number of hospital admissions of patients presenting late diagnosis of cancer added to pre-existing comorbidities. These cases show the need for integral care to prevent or treat complications related to the cancer disease. They may be related to the tumor itself, systemic manifestations of the disease (often the first manifestation of the disease) or side effects of treatment, and may appear in acute or insidious ways, delaying diagnosis and treatment [53]. The term “clinical intercurrence of cancer” is related to a complication of the disease or its treatment, predictable or not, which requires hospitalization in specialized, general or day hospitals, for control of the complication [54]. The procedure “Treatment of Clinical Intercurrences in Oncological Patient” was first published by Decree GM/MS No. 2413, on March 23rd 1998, and was included in the procedures of the Hospital Information System of the Brazilian Health System (SIH-SUS) [54]. Hospitalizations for treatment of clinical intercurrences in oncological patients can be conducted in any hospital, regardless of the authorization for high complexity in oncology. According to the retrospective analysis of hospital admissions data recorded in the Hospital Information System of SUS (SIH-SUS), approximately 90% of the hospital admissions made in the procedure “Treatment of Clinics Intercurrences of Cancer Patient” in Brazil were related to palliative care for terminally ill patients [55-58].
Estimating the needs of palliative care in Brazil
Even though palliative care is traditionally directed to people with cancer, in general it has been very difficult to define the exact number of people with indication of receiving this assistance mode in Brazil and the existing national data have not been processed to estimate the needs in this area. Up to now, the quantification of palliative care needs in our country has been estimated in isolation and based on international experiences. However there are doubts about the applicability of these parameters considering the population and territorial dimensions, as well as the regional diversities [59].
It becomes essential to know the size, nature and severity of the needs of people with regard to access to health services, as well as to identify the availability of resources to promote full assistance in hospice care in our country and, based on models and international studies that consider that, there is 1000 people in need of palliative care, per year, for every 1 million population. We can say that the Brazilian public health policy situation is very delicate, taking into account the size of the population (206 million) and the estimation of health services to meet the needs of 206,000 persons/year [26,60-63]. By analyzing the population morbidity and mortality profile, it becomes necessary to establish feasible parameters to be deployed for assistance in palliative care such as national death register and hospital admissions data for treatment of cancer patients [56]. According to the retrospective analysis of hospital admissions of cancer patients, data recorded in the Hospital Information System of SUS (SIH-SUS), approximately 90% of the hospital admissions made in the procedure “Treatment of Clinics Intercurrences of Cancer Patient” in Brazil were related to palliative care for terminally ill patients [56].
Methodology
Material and methods
This is a cross-sectional study using national death certificate and hospital morbidity and mortality data. The present research has a quantitative approach, with descriptive exploratory, retrospective and observational studies of cancer mortality and hospital admission of cancer patients. Mortality data (2008-2014) was obtained from the Mortality Information System (SIM) in database of DATASUS [57]. Created by the Ministry of Health in 1975, SIM is the oldest nationwide health information system. The National Mortality System is based on death statement information collected by the State Health Departments. The national database generated from this information is administered by the Health Surveillance Secretariat in cooperation with DATASUS. It contains information on the cause of death, as well as sex and age and place of death. The cause of death is coded using the ICD-10-WHO code, making international comparisons possible [64].
Hospital information system (SIH)
Hospital morbidity and mortality data related to cancer were obtained from the Hospital Information System of the Brazilian Health System (SIH-SUS). All hospital admissions for neoplasms occurred in the period (from 2008 to 2014) were included, and hospitalizations that do not fit with the pathology in question were excluded. The entire process of SIH-SUS is based on the Hospital Admission Authorizations (AIH), which includes patient and hospitalization data: description of hospital morbidity and mortality, the benchmarking of hospital assistance, epidemiological surveillance, as well as the validation of other health information systems [65-67]. The records of hospital admissions, hospital beds, hospitals that admitted patients in the procedure “Treatment of Clinical Intercurrences of Oncological Patient,” hospital mortality and overall mortality were obtained from the database of the Health Information Department (DATASUS) of the Ministry of Health, being calculated historical series of residents in Brazil during this period (2008-2014), according to the 10th revision of international classification of diseases (ICD-10). Also, data from 4.5 million hospital admissions of cancer patients registered, between 2008 and 2014, was extracted from Hospital Admission Authorizations (AIH) in Brazil and processed through a system (syntaxes) using Tabwin and SPSS program [52,68-72].
Results
From 2008 to 2014, the Brazilian Health System recorded 78.4 million hospitalizations in public hospitals, including all causes and all age groups, and, of the total admissions registered in that period; 4.4 million admissions (5.6%) were of cancer patients. We also observed, in the same period (2008 to 2014), a variation of 4.4% in the total number of hospitalizations in SUS. There was an increase of 26.7% in hospitalizations related to cancer and 48.1% of hospital admissions for treatment of oncology clinic intercurrences, and, of the total number of hospital admissions (4,431,685) of cancer patients recorded between 2008 and 2014 in the Hospital Information System of SUS, 26.85% (1,189,908) were admitted for treatment of clinical intercurrence of cancer (Table 3).
| Year | Cancer | Clinic intercurrence | ||
| Freq | Rate | Freq | Rate | |
| 2008 | 39,168 | 7.18 | 27,123 | 21.59 |
| 2009 | 44,129 | 7.67 | 32,262 | 22.36 |
| 2010 | 46,937 | 7.76 | 34,104 | 21.93 |
| 2011 | 49,026 | 7.86 | 35,559 | 21.22 |
| 2012 | 51,984 | 7.88 | 38,431 | 20.73 |
| 2013 | 55,340 | 8 | 41,535 | 20.77 |
| 2014 | 57,697 | 7.95 | 43,508 | 20.56 |
| Total | 3,44,281 | 7.77 | 2,52,522 | 21.22 |
Table 3: Hospital admissions in Brazil (2008-2014).
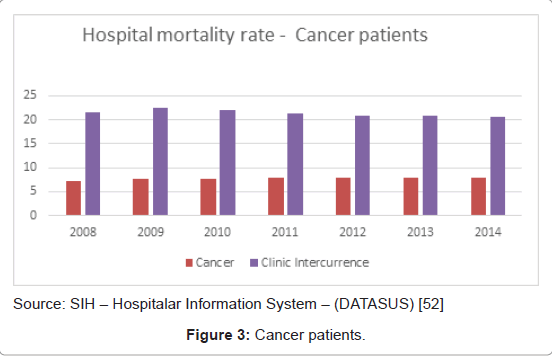
The hospital mortality of cancer patients, as seen in Table 4, was analyzed in frequency and rate. In the period from 2008 to 2014, considering the total number of cancer patients admitted to hospital, the mortality rate among the patients admitted for treatment of clinic intercurrence (21.22) was three times higher than for general cancer (7.77) (Table 4 and Figure 3). In relation to the length of stay (LOS), the patients with cancer as a whole stayed an average of 5.7 days, and the patients admitted for treatment of clinic intercurrence, 7.9 days.
| Year | Cancer | Clinic intercurrence | ||
| Freq | Rate | Freq | Rate | |
| 2008 | 39,168 | 7.18 | 27,123 | 21.59 |
| 2009 | 44,129 | 7.67 | 32,262 | 22.36 |
| 2010 | 46,937 | 7.76 | 34,104 | 21.93 |
| 2011 | 49,026 | 7.86 | 35,559 | 21.22 |
| 2012 | 51,984 | 7.88 | 38,431 | 20.73 |
| 2013 | 55,340 | 8 | 41,535 | 20.77 |
| 2014 | 57,697 | 7.95 | 43,508 | 20.56 |
| Total | 3,44,281 | 7.77 | 2,52,522 | 21.22 |
Table 4: Hospital mortality of cancer patients.
Hospital units with register of oncologic patient admitted for treatment of clinic intercurrence: analysis of data
Study conducted by the authors, through the National Register of Health Establishments-CNES, about hospital resources during the month of December 2014, showed that in Brazil, at that time, whereas the register is updated monthly, there was a total of 6,880 hospitals, being 5,244 (76.2%) general hospitals, 1096 (15.9%) hospitals and specialized hospitals and 540 (7.8%) day- hospitals. In relation to hospital beds, the study presents a total of 452,488 beds, being 319,283 (70.6%) of them beds that belong to SUS and 133,205 (29.4%) beds that do not belong to SUS, including all types of beds: general, specialized, ICU, long stay, day hospital, psychiatric, obstetric, pediatric etc.
Between 2008 and 2014, more than 1 million (1,089,011) hospitalizations for treatment of clinic intercurrence of cancer patients were registered in the Hospital Information System of SUS (SIH-SUS). These admissions were identified on 2,881 different health units around the country, and, of these units, those that had recorded at least 60 admissions per year (5 admissions per month) were identified, resulting in 342 hospitals. In conclusion, between 2008 and 2014, an average of 88% of all hospitalizations for treatment of clinic intercurrence of cancer patient were registered in 342 hospitals (Table 5).
| Year | Hospital admissions of cancer patients for treatment of clinic intercurrence | Number of hospital admitting patients for treatment of clinic intercurrence | Selected hospital with 60 or + admission/year for treatment of clinic intercurrence | Number of cancer patients admitted in selected hospitals (60 or +admission/year) for treatment of clinic intercurrence | Percentage (%)of cancer patients admitted in selectedhospitals for treatment of clinic intercurrence |
| 2008 | 1,14,752 | 1,461 | 327 | 1,02,733 | 90 |
| 2009 | 1,32,459 | 1,606 | 337 | 1,17,419 | 89 |
| 2010 | 1,44,380 | 1,730 | 339 | 1,26,717 | 88 |
| 2011 | 1,55,671 | 1,752 | 342 | 1,38,279 | 89 |
| 2012 | 1,73,320 | 1,776 | 342 | 1,54,039 | 89 |
| 2013 | 1,69,929 | 1,881 | 342 | 1,51,301 | 89 |
| 2014 | 1,98,500 | 1,879 | 339 | 1,72,163 | 87 |
| TOTAL | 10,89,011 | - | - | 9,62,651 | 88 |
Table 5: Hospital admission of cancer patients for treatment of clinic intercurrences.
In the period of 2008 to 2014, an average of 3,066 clinical hospital beds were used for treatment of clinic intercurrence of cancer patients, and, by analyzing the variation of utilization of hospital beds by region, we can say that, in total, there has been an increase of 43.9% of the beds used in the period of 2008 to 2014. The biggest variation occurred in the Northern region (142%), followed by the Southeast (47%) and the Northeast (44.1%), while the smallest variations were observed in the Midwest regions (12.2%) and in the South (29.9%) (Table 6).
| Regions | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Grand Total | Variation |
| Midwest | 123 | 146 | 140 | 119 | 131 | 114 | 138 | 910 | 12.2 |
| Northeast | 490 | 572 | 565 | 555 | 635 | 654 | 706 | 4178 | 44.1 |
| North | 82 | 118 | 142 | 146 | 144 | 145 | 199 | 976 | 142.7 |
| Southeast | 1219 | 1423 | 1481 | 1549 | 1726 | 1692 | 1792 | 10882 | 47.0 |
| South | 571 | 643 | 614 | 639 | 660 | 647 | 742 | 4515 | 29.9 |
| Grand Total | 2485 | 2903 | 2942 | 3008 | 3295 | 3252 | 3577 | 21463 | 43.9 |
Table 6: Clinic hospital beds used for treatment of clinic intercurrence in oncologic patients.
Size of cancer population in need of palliative care
This study was based on estimation models of WHO, Gomez- Batiste, Higginson and Brazilian Parameter of Ministry of Health (MOH) to identify the number of people who were possibly in need of oncologic palliative care. Data on the number and causes of deaths were derived from death registration and hospital admission data.
The following simulations assumed the estimation models of 1) WHO: at least 80% of terminal cancer patients will require palliative care; 2) Gomez-Batiste: 60% of deaths; and 3) Higginson: number of people with selected causes of death (cancer and non-cancer diagnoses), multiplied by standard symptom prevalence (estimated from systematic reviews). Here we used the pain prevalence (Tables 7 and 8) [73-75].
| Year | Total of cancer deaths/year *(A) | Estimating needs of palliative care | ||
| WHO (A*0.8) | Gomez-Batiste(A*0.6) | I.J. Higginson(A*0.84) | ||
| 2008 | 167.677 | 134.142 | 100.606 | 140.849 |
| 2009 | 172.255 | 137.804 | 103.353 | 144.694 |
| 2010 | 178.99 | 143.192 | 107.394 | 150.352 |
| 2011 | 184.384 | 147.507 | 110.63 | 154.883 |
| 2012 | 191.577 | 153.262 | 114.946 | 160.925 |
| 2013 | 196.954 | 157.563 | 118.172 | 165.441 |
| 2014 | 200.979 | 160.783 | 120.587 | 168.822 |
| TOTAL | 1,292.816 | 1,034.253 | 775.69 | 1,085.965 |
WHO: It is assumed that at least 80% of terminal cancerpatients will require palliative care; Gomez-Batiste: 60% of patents at the end-of-life needs palliative care; Higginson: Number of people with selected causes of death (cancer andnoncancer areas), multiplied by standard symptom prevalence (estimated from systematic reviews)
Table 7: Needs of palliative care according to total cancer deaths/year.
| Year | Hospitaladmission Oncologic patient | Hospital death Oncologic patient (A) | Estimating needs of palliative care | ||
| WHO(A*0.8) | Gomez-Batiste(A*0.6) | I J Higginson(A*0.84) | |||
| 2008 | 545.863 | 39.168 | 31334 | 23501 | 32901 |
| 2009 | 575.371 | 44.129 | 35303 | 26477 | 37068 |
| 2010 | 604.809 | 46.937 | 37550 | 28162 | 39427 |
| 2011 | 624.035 | 49.026 | 39221 | 29416 | 41182 |
| 2012 | 659.788 | 51.984 | 41587 | 31190 | 43667 |
| 2013 | 691.543 | 55.34 | 44272 | 33204 | 46486 |
| 2014 | 725.685 | 57.697 | 46158 | 34618 | 48465 |
| TOTAL | 4,427.094 | 344.281 | 275425 | 206569 | 289196 |
WHO: It is assumed that at least 80% of terminal cancerpatients will require palliative care; Gomez-Batiste: 60% of patents at the end-of-life needs palliative care; Higginson: Number of people with selected causes of death (cancer andnoncancer areas), multiplied by standard symptom prevalence (estimated from systematic reviews)
Table 8: Needs of Oncologic Palliative Care According to Hospital Mortality/Year.
The Brazilian studies of MOH estimate that 90% of cancer patients admitted in hospital for treatment of clinic intercurrence should be considered in need of palliative care. This parameter is addressed to morbidity and not mortality (Table 9) [57].
| Year | Hospital admission Clinic intercurrence of oncologic patient (A) | Hospital death Clinic intercurrence of oncologic patient (B) | Estimating needs of palliative care | |||
| WHO (B*0.8) | Gomez-Batiste (B*0.6) | I J Higginson (B*0.84) | Parameter Brazil (A*0.9) | |||
| 2008 | 125.605 | 27.123 | 21.698 | 16.274 | 22.783 | 11.3045 |
| 2009 | 144.302 | 32.262 | 25.81 | 19.357 | 27.1 | 12.9872 |
| 2010 | 155.512 | 34.104 | 27.283 | 20.462 | 28.647 | 13.9961 |
| 2011 | 167.564 | 35.559 | 28.447 | 21.335 | 29.87 | 15.0808 |
| 2012 | 185.406 | 38.431 | 30.745 | 23.059 | 32.282 | 16.6865 |
| 2013 | 199.933 | 41.535 | 33.228 | 24.921 | 34.889 | 17.994 |
| 2014 | 211.586 | 43.508 | 34.806 | 26.105 | 36.547 | 19.0427 |
| TOTAL | 1.189.908 | 25.522 | 202.018 | 151.513 | 212.118 | 1.070.917 |
WHO: It is assumed that at least 80% of terminal cancer patients will require palliative care; Gomez-Batiste: 60% of patents at the end-of-life needs palliative care; Higginson: Number of people with selected causes of death (cancer and noncancer areas), multiplied by standard symptom prevalence (estimated from systematic reviews) MOH - Brazil.
Table 9: Needs of oncologic palliative care according to hospital mortality of clinic intercurrence of oncologic pacient/year.
Comments
The use of health information systems in Brazil allows us to know and to evaluate the process of health management, planning, training of health human resources and health services organization. As they contain demographic, morbidity, mortality and financial data, the use of Hospital Information System (SIH/SUS) have been increasingly exploited by health professionals, mainly by its agility and facility of access.
Even though the use of in-patient data have been aimed at the provision and control of hospital spending, which is the purpose for which it is designed, it is at the same time the only in-patient data source for most states and Brazilian municipalities. Considering the territorial and population dimensions of Brazil, it is necessary to define health coverage parameters to people in need of palliative care.
Through the hospital admissions of cancer patients in the procedure “Treatment of Clinical Intercurrences of Oncological Patients”, we can estimate patients with indication of palliative care at the end of life, as well as identify parameters for the estimated need for cancer palliative care hospital beds. In this regard, we propose studies to size the target population, the demand and supply of health services, the level of attention required by selecting, to that, certain items likely to comparability between national and international data parameters, such as utilization of palliative care services, the prevalence of pain and other symptoms. Also, further study of hospital procedure “Treatment of clinical complications of cancer patient” should be considered as a parameter for scaling of palliative care services in Brazil.
References
- World Health Organization (2014) Strengthening of palliative care as a component of integrated treatment within the continuum of care.
- World Palliative Care Alliance, WHO (2014) Global atlas of palliative care at the end-of-life. Thewpca, London.
- Pan American Health Organization (2007) Regional strategy and plan of action on an integrated approach to the prevention and control of chronic diseases, including diet, physical activity, and health. PAHO, Washington, DC.
- World Health Organization (2007) Cancer control: palliative care. WHO guide for effective programmes. WHO, Geneva.
- The Brazilian Cancer Foudation (2016) Cancer Foundation, Rio de Janeiro, Brazil.
- World Health Organization (2009) Health organization, on behalf of the European Observatory on Health Systems and Policies. WHO, Geneva.
- Index Mundi (2016) Brazil demographic profile 2016.
- Brazilian Institute of Geography and Statistics (2015) Demographic change in Brazil at the beginning of the 21st century: subsidies for the projections of the population of Brazil and of the Federation Units. IBGE, Rio de Janeiro, Brazil.
- Oswaldo Cruz Foundation (2012) Health in Brazil in 2030: guidelines for the strategic prospection of the Brazilian health system. Fiocruz, Rio de Janeiro, Brazil.
- Brazilian Institute of Geography and Statistics (2010) Brazil: Complete mortality table-2010. IBGE, Rio de Janeiro, Brazil.
- Murray SA, Kendall M, Boyd K, Sheikh A (2005) Illness trajectories and palliative care. BMJ 330: 1007-1011.
- Ministry of Health, National Cancer Institute (2006) The cancer situation in Brazil. INCA, Rio de Janeiro, Brazil.
- Ministry of Health, National Cancer Institute (2014) Coordination of prevention and surveillance estimation 2014: incidence of cancer in Brazil. INCA, Rio de Janeiro, Brazil.
- Instituto Oncoguia (2013) When time becomes the enemy of healing.
- Ministry of Health (2014). Ordinance No. 140, of February 27, 2014. MS, Brasília, DF, Brazil.
- Todos juntos contra o câncer (2015)Statement for improving cancer care in Brazil.São Paulo, Brazil.
- Barbosa IR, de Souza DL, Bernal MM, do C C Costa Í (2015) Cancer mortality in Brazil: Temporal Trends and Predictions for the Year 2030. Medicine (Baltimore) 94: e746.
- Felippu AW, Freire EC, Silva Rde A, Guimarães AV, Dedivitis RA (2016) Impact of delay in the diagnosis and treatment of head and neck cancer. Braz J Otorhinolaryngol 82: 140-143.
- Freitas AGQ, Weller M (2015) Patient delays and system delays in breast cancer treatment in developed and developing countries. Cien Saude Colet. 20: 3177-3189.
- Santos CL, Mattos LF (2011) Palliative care and family and community medicine. In: Santana F, editor. Palliative care: guidelines, humanization and symptom relief. Atheneu, São Paulo, Brazil, pp: 17-24.
- Sinsuwan W, Pairojkul S, Gomutbutra P, Kongkum K, Kosuwon W (2016). A retrospective, single center, observational study, comparing the direct cost of end-of-life care patients with advanced cancer care: palliative care versus usual care. J Palliat Care Med 6: 243.
- Figueiredo TA (2006) Reflections on palliative care in Brazil. Prat Hosp 47: 36-40.
- Ling J (2010) Ranking palliative and end-of-life care. Int J Palliat Nurs 16: 367.
- Wright M1, Wood J, Lynch T, Clark D (2008) Mapping levels of palliative care development: a global view. J Pain Symptom Manage 35: 469-485.
- Shetty P (2010) The parlous state of palliative care in the developing world. Lancet 376: 1453-1454.
- Gomez-Batiste X, Porta-Sales J, Tuca A, Stjernsward J (2005) Organization of Palliative Care Services and Programs. Aran, Madrid.
- Twycross R (2003) Palliative care. (2nd edn.) Climepsi, Lisboa.
- Floriani CA (2008) Palliative care in Brazil: a challenge to the health-care system. Palliat Care Res Treat 2: 19-24.
- Irish Hospice Foundation (2008) Palliative care for all: integrating palliative care into disease management frameworks. IHF, Dublin.
- Garcia JBS, Rodrigues RF, Lima SF. Structuring a palliative care service in Brazil: experience report. (2014) Rev Bras Anestesiol 64: 286-291.
- Brasil (2010) Constitution of the Federative Republic of Brazil: constitutional text of October 5, 1988, with the alterations introduced by Constitucional Amendments no. 1/1992 through 64/2010 and by Revision Constitutional Amendments no. 1/1994 through 6/1994. (3rd edn.) Chamber of Deputies, Documentation and Information Center, Brasília, DF, Brazil.
- Brazilian Institute of Geography and Statistics (2011) Population. IBGE, Rio de Janeiro, Brazil.
- Paim J, Travassos C, Almeida C, Bahia L, Macinko J (2011) The Brazilian health system: history, advances, and challenges. Lancet 377: 1778-1797.
- Ministry of Health (1993) Portaria SAS / MS n° 65/93: establishes norms for accreditation of hospitals that perform procedures of high complexity in Cancer. MS, Brasília, DF, Brazil.
- Ministry of Health (1998) Ordinance No. 2,413, dated March 23, 1998. Care for patients under long-term care. MS, Brasília, DF, Brazil.
- Ministry of Health (1998) Portaria No. 3.535 / GM, of September 02, 1998. Criteria for registration of centers of attendance in oncology. MS, Brasília, DF, Brazil.
- Brazilian Institute of Geography and Statistics (2000) Profile of the elderly responsible for the households in Brazil. IBGE, Rio de Janeiro, Brazil.
- Ministry of Health (2002) Portaria GM / MS No. 19, of January 3, 2002. Establishes the National Program of Assistance to Pain and Palliative Care of the Unified Health System - SUS. MS, Brasília, DF, Brazil.
- Ministry of Health (2005) GM / MS Ordinance No. 2,439, of December 8, 2005. Establishes the national policy of cancer care: promotion, prevention, diagnosis, treatment, rehabilitation and palliative care. MS, Brasília, DF, Brazil.
- Ministry of Health (2006) Ordinance MS / GM No. 2528, of October 20, 2006. National health policy of the elderly.MS, Brasília, DF, Brazil.
- Malta DC, Oliveira TP, Santos MA, Andrade SS, Silva MM; Grupo Técnico de Monitoramento do Plano de DCNT (2016) Progress with the Strategic Action Plan for Tackling Chronic Non-Communicable Diseases in Brazil, 2011-2015. Epidemiol Serv Saude 25: 373-390.
- Ministry of Health (2013) Ordinance No. 874 / GM / MS, of May 16, 2013. Establishes the national policy of prevention and control of cancer in the health care network of people with chronic diseases under the SUS. MS, Brasília, DF, Brazil.
- Ministry of Health (2014) GM / MS Ordinance No. 483, of April 1, 2014. Redefines the health care network of people with chronic diseases under the Unified Health System (SUS) and establishes guidelines for the organization of their care lines. Brazil.
- Ministry of Health (2005) GM / MS Ordinance No. 2,439 / 2005. It establishes the national cancer care policy: promotion, prevention, diagnosis, treatment, rehabilitation and palliative care, to beimplemented in all the federated units, respecting the competences of the three management spheres. MS, Brasília, DF, Brazil.
- Ministry of Health (2005) Surveillance, control and prevention of chronic non-communicable diseases: CNCD in the context of the Brazilian Unified Health System. MS; Brasília, DF, Brazil.
- De Lima L, Wenk R, Krakauer E, Ferris F, Bennett M, et al. (2013) Global framework for noncommunicable diseases: how can we monitor palliative care? J Palliat Med 16: 226-229.
- World Health Organization (2013) Health topics: chronic diseases. WHO, Geneva.
- Pan American Health Organization (2014) Plan of action for the prevention and control of noncommunicable diseases in the Americas: 2013-2019. PAHO, Washington, DC.
- World Health Organization (2014) Global status report on noncommunicable diseases. WHO, Geneva.
- Ministry of Health (2016) SIM -Mortality Information System. DATASUS, Brasília, DF, Brazil.
- National Cancer Institute José Alencar Gomes da Silva (2014) Cancer in Brazil: data from the population-based registries (v.4). INCA, Rio de Janeiro, Brazil.
- Ministry of Health (2013) SIHSUS: SUS hospital information systems. DATASUS, Brasília, DF, Brazil.
- Lorite JCP (2009) I manage serious complications in cancer patients. Department of Obstetrics and Gynecology, University Hospital Virgen de las Nieves, Granada.
- Ministry of Health (2013) Oncology Technical Basis Manual. (16th edn.) MS, Brasília, DF, Brazil.
- Ministry of Health (2013) Technical manual of the hospital information system: technical guidelines, 2010. MS, Brasília, DF, Brazil.
- Ministry of Health (2015) Oncology technical basis manual- SIA/SUS - outpatient information system. (19th edn.), MS, Brasília, DF, Brazil.
- Maciel MGS, Rodrigues LF, Naylor C, Bettega R, Barbosa SM, et al. (2006) Critérios de qualidade para os cuidados paliativos no Brasil. Diagraphic, Rio de Janeiro, Brazil.
- Santos CE, Caldas JMP, Serafim JA, Barros N, Pereira AC (2016) Hospital admissions of cancer patients in brazil: analysis of palliative care needs. J Palliat Care Med 6: 263.
- Brameld K, Spilsbury K, Rosenwax L, Murray K, Semmens J (2016) Issues using linkage of hospital records and death certificate data to determine the size of a potential palliative care population. Palliat Med.
- Maciel MGS (2009) Organization of palliative care services. In: National Academy of Palliative Care. Manual of palliative care. Diagraphic, Rio de Janeiro, Brasil.pp: 72-85.
- Stjernswärd J, Foley KM, Ferris FD (2007) The public health strategy for palliative care. J Pain Symptom Manage 33: 486-493.
- McNamara B, Rosenwax LK, Holman CD (2006) A method for defining and estimating the palliative care population. J Pain Symptom Manage 32: 5-12.
- Bittencourt SA, Camacho LAB, Leal MC (2006) The hospital information system and its application in collective health. Cad Saude Publica 22: 19-30.
- Lima EEC, Queiroz BL (2014) Evolution of the deaths registry system in Brazil: associations with changes in the mortality profile, under-registration of death counts, and ill-defined causes of death. Cad Saúde Pública 30: 1721-1730.
- Amaral TCL (2002) Health information systemsMortality in the SUS network: mirror of the deaths occurred in the Brazilian population? [thesis]. University of the State of Rio de Janeiro, Rio de Janeiro, Brazil.
- Sanches KRB, Camargo KR, Coeli CM, Cascão AM (2003) Health Information Systems. In: Medronho RA, Carvalho DM, Block KV, Luiz RR, Werneck GL, organizadores. Epidemiologia Atheneu, São Paulo, Brazil, pp:337-359.
- Ministry of Health. National Cancer Institute (2016) Cancer statistics. INCA, Brasília, DF, Brazil.
- Brazilian Institute of Geography and Statistics (2016) Mortality Information System (SIM). IBGE, Rio de Janeiro, Brazil.
- Ministry of Health (2008) Health information (TABNET). MS, Brasília, DF, Brazil.
- Gragnolati M, Lindelow M, Couttolenc B (2013) Twenty years of health system reform in Brazil: an assessment of the Sistema Único de Saúde. The World Bank, Washington, DC.
- Ministry of Health (2016) Mortality information system. Brazil.
- Teixeira CLS, Bloch KV, Klein CH, Coeli CM (2006) Method of relationship of databases of the Mortality Information System and authorizations of hospital admission in the Unified Health System, in the investigation of deaths of ill-defined cause in the State of Rio de Janeiro, Brazil, 1998. Epidemiol Serv Saúde 15: 47-57.
- World Health Organization (2007) Cancer control: knowledge into action: WHO guide for effective programmes; module 5. WHO, Geneva.
- Gomez-Batiste X, Martínez-Muñoz M, Blay C, Espinosa J, Contel JC, et al. (2012) Identifying needs and improving palliative care of chronically ill patients: a community-orientated, population-based, public health approach. Curr Opin Support Palliat Care 6: 371-378.
- Higginson IJ (1997) Palliative and terminal care healthcare needs assessment: the epidemiologically based needs assessment reviews. The Wessex Institute for Health Research and Development , Oxford.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 3690
- [From(publication date):
January-2017 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 2776
- PDF downloads : 914