Opinion Article Open Access
Percutaneous Transesophageal Gastro-tubing: A New Treatment Strategy for Gastric Leakage after Sleeve Gastrectomy
Oshiro T1*, Oishi H2, Okazumi S1 and Katoh R11Department of Surgery, Toho University Medical Center, Sakura Hospital, Japan
2Department of Surgery, Murayama Medical Center, National Hospital Organization, Japan
- *Corresponding Author:
- Takashi Oshiro
Department of Surgery, Toho University Medical Center
Sakura Hospital, 564-1 Shimoshizu, Sakura, Chiba, 285-8741, Japan
Tel: 043-462-8811
Fax: 043-462-8820
E-mail: oshiro@sakura.med.toho-u.ac.jp
Received date: June 09, 2017; Accepted date: June 14, 2017; Published date: June 19, 2017
Citation: Oshiro T, Oishi H, Okazumi S, Katoh R (2017) Percutaneous Transesophageal Gastro-tubing: A New Treatment Strategy for Gastric Leakage after Sleeve Gastrectomy. J Obes Weight Loss Ther 7: 342. doi:10.4172/2165-7904.1000342
Copyright: © 2017 Oshiro T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Obesity & Weight Loss Therapy
Abstract
The number of laparoscopic sleeve gastrectomy (LSG) performed worldwide is increasing continuously. Serious complications are relatively rare, but staple line leakage after LSG remains one of the most dreaded acute complications. Endoscopic treatments play a major role in treating sleeve leakage after initial surgical or percutaneous perigastric abscess control. Despite the high success rate of endoscopic treatments, some patients who fail treatment can develop refractory chronic leakage or fistula; therefore, they require revision operation such as Roux-en-Y gastric bypass or even total gastrectomy. We herein comment on percutaneous transesophageal gastro-tubing (PTEG) as a non-endoscopic, non-surgical alternative treatment option in patients for whom it may be desirable to avoid complex reoperation for sleeve leakage.
Keywords
Laparoscopic sleeve gastrectomy; Complications; Sleeve leakage; Over-the-scope-clip; Stent; Percutaneous transesophageal gastro-tubing
Opinion Article
Although a linear stapler has been improved to complete a required task, staple line leakage is one of the troublesome complications after sleeve gastrectomy. An endoscopic approach, such as an Over-The- Scope-Clip (OTSC®, Ovesco Endoscopy, Tübingen, Germany) or stent, has become a valid treatment option for acute sleeve leakage [1].
The OTSC® system offers the advantage of a nitinol clip loaded at the tip of the endoscope that can capture the leak and fistula orifice and compress them constantly until they are healed. This system is gaining popularity as a reliable option for treating leakage after sleeve gastrectomy [2]. Despite the high success rate for closure of sleeve leakage, surgeons must realize the limitation of this method. Difficulties may arise in the treatment of a chronic leak or fistula, which is surrounded by hardened and inelastic tissues unfit to be approached endoscopically. Fibrotic tissue is rigid and difficult to suction or pull into the applicator cap. Care must also be taken to avoid laceration in cases of larger leaks [3].
Endoscopic stenting is one of the most well-established, viable options for treating sleeve leakage [4]. Endoluminal stenting has the advantages of being able to cover the leak site and to correct gastric tube stenosis and axis deviation simultaneously. However, the main concerns with stents are migration and insufficient sealing. Although a tailored mega stent would be a possible solution for these problems, it is not yet widely available [5]. Another disadvantage of stenting is that the stent is positioned at the gastroesophageal junction for proximal leaks, which are most commonly observed; thus, patients can develop unendurable symptoms, such as nausea, vomiting, and retrosternal discomfort. Therefore, stenting is not always a universally acceptable treatment at present.
Revision operation must be regarded as a last resort if endoscopic approaches fail. Total gastrectomy (open or laparoscopic) is a practical approach for a chronic leak or fistula; however, it has a high morbidity rate, and it is technically demanding to perform [6,7]. In addition, surgeons should recognize potential future problems, including an iron deficiency or pernicious anemia and a complicated access to the biliary tract after total gastrectomy
We believe that percutaneous transesophageal gastro-tubing (PTEG) should be considered when revision operation is the only remaining option for intractable sleeve leaks. PTEG was originally developed as a feasible alternative to nasogastric decompression in patients unsuitable for percutaneous endoscopic gastrostomy using the transesophageal approach [8]. Its characteristics can be practically applied in the treatment of leakage after a gastrointestinal operation. As we previously reported, PTEG can serve the dual purposes of splinting the leakage site and providing jejunal nutritional access during the management of sleeve leakage near the esophagogastric junction [9].
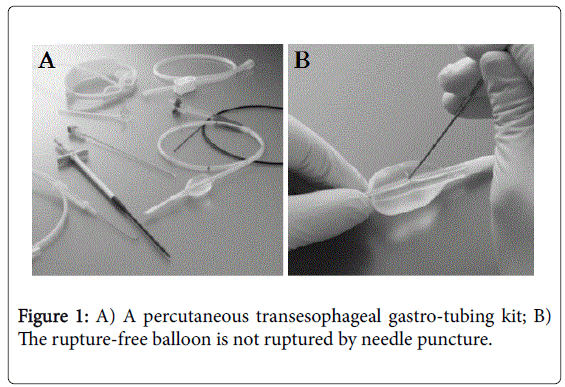
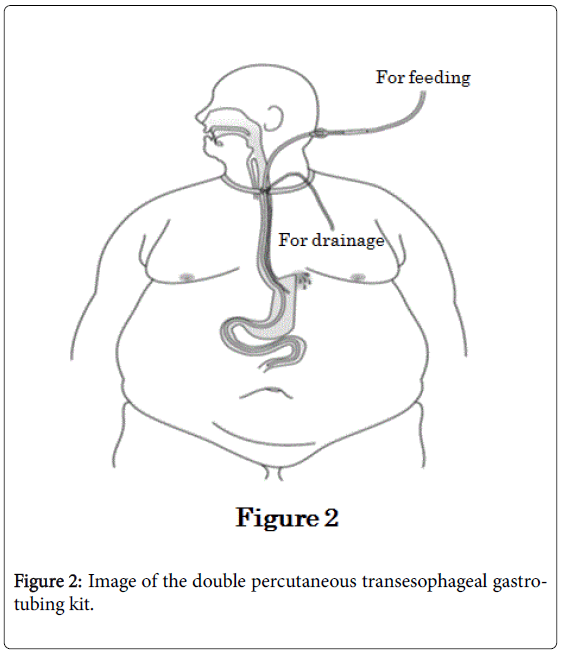
The PTEG kit (Sumitomo Bakelite Co., Ltd., Tokyo, Japan) includes ready-to-use devices, such as a needle with a sheath, rupture-free balloon (RFB), dilator, guidewires and long placement tube (Figure 1). In brief, the procedure is performed as follows. An RFB is dilated with contrast medium mixed with saline in the upper esophagus to facilitate percutaneous esophageal puncture under ultrasonography and fluoroscopy. A matching guidewire is threaded into the esophageal lumen through an introducer needle. After dilating the path around the guidewire, the indwelling tube is advanced over the guidewire. Furthermore, double PTEG was invented to provide an additional intraluminal tube through the same opening of the primary PTEG using a second guidewire and a dilator with a peel-away sheath. Double PTEG can simultaneously attain enteral nutrition access and gastrointestinal decompression separately through each tube (Figure 2). Unlike a nasogastric tube through the nostril, double PTEG is suitable for long-term purposes secondary to poor tolerability of a nasogastric tube.
Both procedures have been performed under local anesthesia and/or intravenous sedation with no severe adverse events [10]. Bleeding and stomal leakage are rare but potential complications after these procedures. However, gentle dilation of the stoma with a rotating motion can minimize localized bleeding. Even if bleeding occurs after the procedure, hemostasis can be achieved by applying external pressure at the site, following complete removal of the tube [8]. Regarding stomal leakage, the subcutaneous thickness and angled insertion of the tube into the esophagus may lessen the probability of occurrence, especially in obese patients [9]. Nevertheless, surgeons should be well aware of contraindications to double PTEG. The procedure is contraindicated in patients with coagulopathy, right recurrent nerve paralysis, and pathologic conditions in or around the cervical esophagus [8].
PTEG may be a minimally invasive, effective alternative in patients with sleeve leakage. It can also be a potential non-endoscopic, nonsurgical approach to leakage after a gastrointestinal operation, such as Roux-en-Y gastric bypass and total gastrectomy.
References
- Rached AA, Basile M, El Masri H (2014) Gastric leaks post sleeve gastrectomy: Review of its prevention and management. World J Gastroenterol 20: 13904-13910.
- Shoar S, Poliakin L, Khorgami Z, Rubenstein R, El-Matbouly M, et al. (2017) Efficacy and safety of the over-the-scope clip (OTSC) system in the management of leak and fistula after laparoscopic sleeve gastrectomy: A systematic review. Obes Surg.
- Sulz MC, Bertolini R, Frei R, Semadeni G, Borovicka J, et al. (2014) Multipurpose use of the over-the-scope-clip system ("Bear claw") in the gastrointestinal tract: Swiss experience in a tertiary center. World J Gastroenterol 20: 16287-16292.
- Galloro G, Ruggiero S, Russo T, Telesca AD, Musella M, et al. (2015) Staple-line leak after sleve gastrectomy in obese patients: A hot topic in bariatric surgery. World J Gastrointest Endosc 7: 843-846.
- Shehab HM, Hakky SM, Gawdat KA (2016) An endoscopic strategy combining mega stents and over-the-scope clips for the management of post-bariatric surgery leaks and fistulas (with video). Obes Surg 26: 941-948.
- Bruzzi M, Douard R, Voron T, Berger A, Zinzindohoue F, et al. (2016) Open total gastrectomy with Roux-en-Y reconstruction for a chronic fistula after sleeve gastrectomy. Surg Obes Relat Dis 12: 1803-1808.
- Ramos AC, Ramos MG, Campos JM, Galvão NMP, Bastos EL (2015) Laparoscopic total gastrectomy as an alternative treatment to postsleeve chronic fistula. Surg Obes Relat Dis 11: 552-556.
- Oishi H, Shindo H, Shirotani N, Kameoka S (2003) A nonsurgical technique to create an esophagostomy for difficult cases of percutaneous endoscopic gastrostomy. Surg Endosc 17: 1224-1227.
- Oshiro T, Saiki A, Suzuki J, Satoh A, Kitahara T, et al. (2014) Percutaneous transesophageal gastro-tubing for management of gastric leakage after sleeve gastrectomy. Obes Surg 24: 1576-1580.
- Udomsawaengsup S, Brethauer S, Kroh M, Chand B (2008) Percutaneous transesophageal gastrostomy (PTEG): A safe and effective technique for gastrointestinal decompression in malignant obstruction and massive ascites. Surg Endosc 22: 2314-2318.
Relevant Topics
- Android Obesity
- Anti Obesity Medication
- Bariatric Surgery
- Best Ways to Lose Weight
- Body Mass Index (BMI)
- Child Obesity Statistics
- Comorbidities of Obesity
- Diabetes and Obesity
- Diabetic Diet
- Diet
- Etiology of Obesity
- Exogenous Obesity
- Fat Burning Foods
- Gastric By-pass Surgery
- Genetics of Obesity
- Global Obesity Statistics
- Gynoid Obesity
- Junk Food and Childhood Obesity
- Obesity
- Obesity and Cancer
- Obesity and Nutrition
- Obesity and Sleep Apnea
- Obesity Complications
- Obesity in Pregnancy
- Obesity in United States
- Visceral Obesity
- Weight Loss
- Weight Loss Clinics
- Weight Loss Supplements
- Weight Management Programs
Recommended Journals
Article Tools
Article Usage
- Total views: 4573
- [From(publication date):
June-2017 - Sep 01, 2025] - Breakdown by view type
- HTML page views : 3712
- PDF downloads : 861