Short Communication Open Access
Plasma Exchange for Autoimmune Encephalitis and Acute Demyelinating Encephalomyelitis in Children: Clinical and Radiological Characteristics
T Moussa1, L Baker1, A Chehab1, H Osman1, A Elbeltagi2, A Kaddourah3, A Khair1 and K Mohamed1*
11Department of Paediatric Neurology, Hamad General Hospital, Qatar
22Department of Neuro-radiology, Hamad General Hospital, Qatar
33Department of Nephrology, Hamad General Hospital, Qatar
- *Corresponding Author:
- Khalid A Mohamed
Department of Paediatric Neurology
Hamad General Hospital, Qatar
Tel: 901-287-6303
E-mail: KMohamed9@hamad.qa
Received Date: September 06, 2017 Accepted Date: September 26, 2017 Published Date: September 28, 2017
Citation: Moussa T, Baker L, Chehab A, Osman H, Elbeltagi A, et al. (2017) Plasma Exchange for Autoimmune Encephalitis and Acute Demyelinating Encephalomyelitis in Children: Clinical and Radiological Characteristics. J Neuroinfect Dis 8: 262. doi: 10.4172/2314-7326.1000262
Copyright: © 2017 Moussa T, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Autoimmune encephalitis (AE) is a term used to indicate onset of acute neuropsychiatric symptoms with deterioration of consciousness, seizures and focal neurological deficit secondary to a presumed autoimmune aetiology. Infections such as acute bacterial or viral encephalitis, toxins and other causes of encephalopathy should be excluded. Additionally, a search for an aetiological factor should include testing blood and CSF for the likely causative antibodies.
Keywords
Autoimmune encephalitis; Plasma exchange; Intra-venous immune globulins
Introduction
The clinical spectrum is wide and includes Limbic Encephalitis (LE) and Neuro-myelitis optica among a wide variety of clinical syndromes while the aetiological factors are also diverse and include some of the known antibodies such as Anti-N-methyl-D-aspartate NMDAR antibodies and Voltage Gated Potassium Channel (VGKC). In children with AE the chance of finding antibodies is around 33% as reported by Gable et al in a large cohort of patients in California [1].
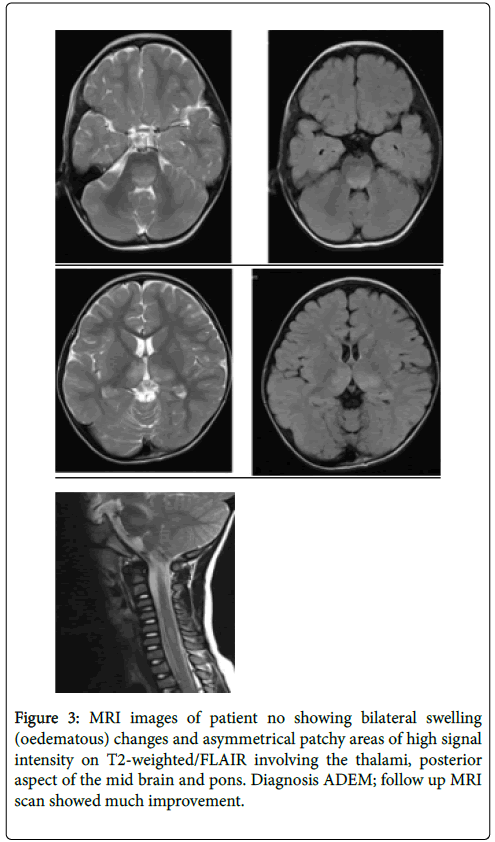
Acute demyelinating encephalomyelitis (ADEM), on the other hand, is an acute onset encephalopathy associated with multifocal neurologic deficits with evidence of demyelination in the brain or spinal cord involving predominantly but not exclusively the white matter, autoantibodies are usually negative in ADEM although some patients demonstrate anti MOG antibodies as a transient feature with ADEM [2].
Following initial resuscitation and exclusion of central nervous system infections, immune therapy in the form of corticosteroids, immunoglobulins or plasma exchange is the standard first line treatment for both AE and ADEM.
Plasma Exchange (PE) is an extracorporeal intervention designated to exchange patient’s plasma containing the presumptive causative antibodies or toxins with physiologic fluids or plasma.
Plasma exchange has been proven to be a valuable immune modulator in a number of auto-immune conditions including neurological disorders of auto-immune origin. A recent review from our institution Khair [3] reviewed the common uses of this modality in autoimmune encephalitis and several practice guidelines have been developed to help establish and evidence base for the use of this therapy in children with neurological disorders [4,5].
In the study we present the clinical presentation and the radiological and laboratory findings of all children who underwent PE for either auto-immune encephalitis or acute demyelinating encephalomyelitis, children who required PE for ADEM were either on the severe end of the spectrum or failed to respond to the first line therapy with methylprednisolone or Intra-Venous Immune Globulins (IVIG).
Methods
This is a retrospective case series study of all patients who received PE for immune mediated encephalopathy (AE or ADEM) at our institution between 2013-2016 all pediatric patients who received such treatment in the state of Qatar were captured in this study.
Patients
Patients were selected for the treatment based on their clinical presentation; patients with prolonged disease may have had more than one session of plasmapheresis.
Clinical and radiological criteria were used to differentiate between AE and ADEM based on the onset of disease and the location and nature of the imaging abnormalities (Table 1).
Technique of plasma exchange
All plasma exchanges were conducted using the Spectra Optia® apheresis system (Terumo Co). The exchanges were universally done using 5% albumin unless there was an evidence of potential coagulopathy where fresh frozen plasma (FFP) were used. Plasma volume exchanges ranged between 1-1.5 of calculated plasma volume.
Statistics
Descriptive with T student test for statistical analysis.
Results
14 patients (8 males) received plasmapheresis for AE and ADEM in the study period, 8 patients (5 males) were diagnosed with probable AE and 6 patients (3 males) with probable ADEM based on the clinical and radiological pictures as detailed above. Age range between 14 months and 8 years (mean: 4.5 years).
All patients presented with altered sensorium (the clinical presentation is detailed in Table 1).
| Clinical symptoms/signs | Patients with AE (8) | Patients with ADEM (6) |
|---|---|---|
| Altered consciousness | 7 | 6 |
| Fever | 6 | 4 |
| Seizures (focal) | 5 (3) | 2 (0) |
| Abnormal movements | 7 | 1 |
| Behavioral changes | 7 | 2 |
| Weakness (inability to walk) | 6 | 5 |
| Swallowing and speech difficulties | 2 | 0 |
| Others (facial palsy, tics) | 2 | 0 |
Table 1: The clinical presentation is detailed.
Of the AE patients only two out of the eight patients had a normal outcome and five had at least mild learning problems and four had epilepsy. In the patients with ADEM Four out of the six had a normal outcome, two had moderate motor difficulties and no patient had epilepsy.
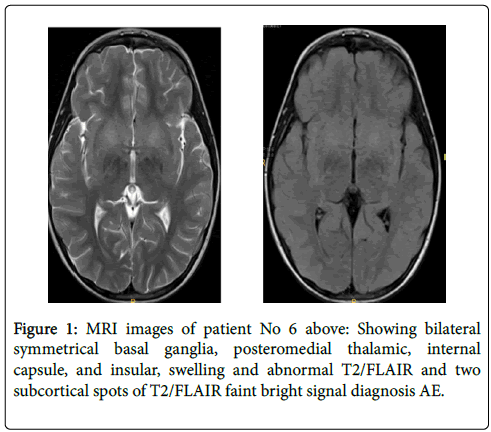
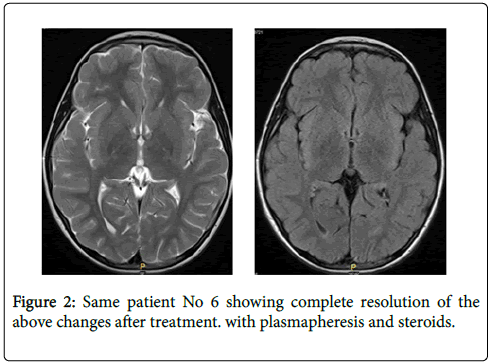
All patients underwent MRI imaging and 11 out of the 12 patients CSF studies; one patient had 2 LPs and two patients had three (Figures 1-3).
Discussion
The incidence of AE is estimated to be around 0.85/million annually based on a study from China [6,7]; this was also replicate din the UK surveillance study that identified 39 children with AE positive for NMDAR which is by large the commonest antibody in this group of children so the overall incidence maybe a bit higher than 0.85 [8]; working on an estimated population of 300.000 children in Qatar; we have 3 antibody confirmed cases of AE in 3 years which makes the incidence around 3.3 per million which is much higher than the rate the literature suggest the large California encephalitis study (Gable) 1 reported a high incidence on NMDAR encephalitis but does not report a community based incidence and there are various reports that suggest there is a high incidence of NMDAR in HSV encephalitis.
We have not included the antibody negative suspected cases in the incidence data and we excluded neuromyelitis optica as a separate aetiology.
This may be related to a combination of genetic and environmental factors and may lead to a better understanding of the aetiology of such conditions.
Our data supports the growing evidence that plasmapheresis is a promising modality of immunotherapy for patients with severe ADEM and AE; to be effective Plasmapheresis should be considered as soon as the first line of therapy does not produce a significant improvement.
There has been increasing evidence for the benefit from plasma exchange is effective in peripheral nervous system disorders such as Gullian Barre syndrome and a recent systematic review by Chevret et al. concluded that plasma exchange speeds the rate of recovery and probably increases the chance of complete muscle strength recovery after one year [9].
In central nervous system disorders a review by Andrews et al. demonstrated a dramatic and consistent response to plasmapheresis in 4 patients with Rasmussen’s syndrome, a classic example of a central nervous system autoimmune disorder [10]; this was replicated in other studies in other autoimmune CNS disorders including several case reports suggesting a rapid response to treatment with PE in such patients [11].
We are using plasmapheresis earlier in patients with AE and severe ADEM and in younger children to the age of 14 months this poses technical challenges but the younger children tended to respond better.
It is not surprising that children with ADEM do much better than children with AE; the outcome of AE depends mostly on the aetiological factors and even though there is a temporary improvement with immune therapy the prognosis is generally guarded.
We observed improvement in both groups within 72 hours of plasmapheresis, this improvement was sustained in 5 out of the 6 patients with ADEM but only 3 out of the 8 with AE the other 5 ended up with motor difficulties and epilepsy in addition to learning difficulties as detailed in Table 2. We followed up three patients for over 2 years and there was slow but continuing improvement with rehabilitation.
| Patient No | MRI findings | CSF findings | Diagnosis/Aetiology | Outcome |
|---|---|---|---|---|
| 1 | Normal twice | 1st LP 21 cells normal Protein antibodies negative | AE (cause unknown) | Full recovery |
| 2 | Normal twice | 10 WBC, normal protein, antibodies negative | AE (Streptococcal related) ASOT 1000 s | Behavioural and learning problems |
| 3 | Normal once | NA | AE unknown cause | Full recovery |
| 4 | Abnormal bilateral enhancement of the temporal lobe/hippocampus | 2 WBC normal protein | AE (NMDAR Positive) | Mild learning problems and epilepsy |
| 5 | Extensive involvement of the thalami and basal ganglia | 23 WBC and protein 0.5 g/l autoantibodies negative | AE (Acute necrotizing encephalitis) cause unknown | Severe neuro deficit and epilepsy |
| 6 | White matter and basal ganglia changes | 33 WBC protein 0.74 g/l Autoantibodies negative |
AE probably secondary to viral encephalitis | Moderate learning and behavioural difficulties/epilepsy |
| 7 | Meningeal enhancement consistent with acute infection, 2nd MR normal | 458 WBC Protein 1 g/l EBV positive and NMDAR abs positive |
AE (NMDAR positive) | Epilepsy and learning difficulty |
| 8 | White matter changes with high signal and oedema | 11 WBC; Protein 0.2 g/l autoantibodies negative | AE (positive for GAD antibodies in the blood) | Full recovery |
Table 2: Imaging and CSF Details the 8 patients with AE.
Our data is hospital based but all symptomatic patients with AE are admitted to this single referral centre.
This study is limited by the nature of the study design being observational and retrospective. Definite conclusions cannot be extracted. The results certainly call for further research to define this role better.
However, we have confirmed the utility of Plasma exchange in the acute management of both ADEM and AE and we have estimated the incidence of AE in the state of Qatar. Further prospective work is underway to understand the natural history of AE and the role of plasma exchange in its acute management.
Conclusion
AE is relatively common in Qatar. Plasmapheresis appears to be of benefit for children with severe ADEM and AE and warrants early consideration. Further research is needed to define the role of this therapy and develop evidence based clinical guidelines.
References
- Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA (2012) The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the california encephalitis project. Clin Infect Dis 54: 899–904.
- Pröbstel AK, Dornmair K, Bittner R, Sperl P, Jenne D, et al (2011) Antibodies to MOG are transient in childhood acute disseminated encephalomyelitis. Neurology 77: 580-588.
- Khair AM (2016) Utility of plasmapheresis in autoimmune-mediated encephalopathy in children: Potentials and challenges neurology research international 2016: 7.
- Szczepiorkowski ZM, Winters JL, Bandarenko N, Kim HC, Linenberger ML, et al. (2010) Guidelines on the use of therapeutic apheresis in clinical Practice: Evidence-based approach from the apheresis applications committee of the American Society for Apheresis. J Clin Apher 25: 83–177.
- Cortese I, Chaudhry V, So YT, Cantor F, Cornblath DR, et al. (2011) Evidence-based guideline update: plasmapheresis in neurologic disorders: Report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology 76: 294–300.
- Latimer ME, Etoile NL, Seidlitz J, Swedo SE (2015) Therapeutic plasma apheresis as a treatment for 35 severely ill children and adolescents with pediatric autoimmune neuropsychiatric disorders associated with Streptococcal infections. J Child Adoles Psychopharmacol 25: 70–75.
- Guan HZ, Ren HT, Cui HY (2016) Autoimmune encephalitis: An expanding frontier of neuroimmunology. Chin Med J Engl129: 1122–1127.
- Wright S, Hacohen Y, Jacobson L, Agrawal S, Gupta R, et al. (2015) N-methyl-D-aspartate receptor antibody-mediated neurological disease: Results of a UK-based surveillance study in children. Arch Dis Child 100: 521-526.
- Chevret S, Hughes RAC, Annane D (2016) Plasma exchange for Guillain-Barré syndrome Cochrane Library Databases. Neuromuscular Group.
- Andrews PI, Dichter MA, Berkovic SF, Newton MR, McNamara JO (1996) Plasmapheresis in Rasmussen's encephalitis. Neurology 46: 1 242-246.
- Nunez-Enamorado N, Camacho-Salas A, Belda-Hofheinz S, Cordero-Castro C, Simon-De Las Heras R, et al. (2012) Fast and spectacular clinical response to plasmapheresis in a paediatric case of anti-NMDA encephalitis. Rev Neurol 54: 420-424.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 6736
- [From(publication date):
September-2017 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 5805
- PDF downloads : 931