Case Report Open Access
Racemose Neurocysticercosis with Psychiatric Symptoms: A Case Report
Fabiano Reis*, Lisiane Seguti Ferreira and Luciano de Souza Queiroz
Faculty of Medical Sciences, Department of Radiology, State University of Campinas, Brazil
- *Corresponding Author:
- Fabiano Reis
Faculty of Medical Sciences
Department of Radiology
State University of Campinas, Brazil
Tel: +81 3061-6479
E-mail:fabianoreis2@gmail.com
Received June 25, 2014; Accepted September 10, 2014; Published September 18, 2014
Citation: Reis F, Ferreir, De Souza Queiroz L, (2014) Racemose Neurocysticercosis with Psychiatric Symptoms: A Case Report. J Neuroinfect Dis 6:163. doi:10.4172/2314-7326.1000163
Copyright: © 2014 Reis F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Background: Neurocysticercosis (NCC) is the most common parasitic disease of the central nervous system and a serious public health problem. NCC is polymorphic and epilepsy is the most common manifestation, followed by headache, focal signs and intracranial hypertension. Psychiatric disorders are less frequent and may include depression, psychotic symptoms and even severe dementia.
Purpose: DThis paper describes the case of a patient with racemose NCC and psychiatric symptoms. A discussion is also offered on neuroimaging findings of this uncommon form of presentation.
Methods: SA 39-year-old male patient presented with a two-month history of disorientation. The diagnosis was suggested by computerized tomography and magnetic resonance, the images of which were compatible with racemose NCC.
Conclusions: Rapid diagnosis and prompt treatment allowed the complete resolution of the psychiatric symptoms and regression of the lesions. These findings demonstrate the decisive role of neuroradiology in such cases.
Keywords
Neurocysticercosis; Racemose; Psychiatric; Organic mental disorders.
Background
Neurocysticercosis (NCC) is the most common parasitic disease of the central nervous system and public health problem that is the major cause of late-onset epilepsy in endemic areas [1-3]. The literature reports an incidence of 1.5% in autopsies and 3.0% in clinical studies. However, prevalence rates are underestimated due mainly to negligence regarding mandatory notification and difficulties in performing imaging exams [4]. NCC is polymorphic and epilepsy is the most common manifestation (70 to 90% of cases), followed by headache (38%), focal signs (16%) and intracranial hypertension (12%). Other manifestations are found in less than 10% of cases [1,5]. Clinical status depends on the number, type, location and development stage of the cysticerci as well as the host immune response to the parasite [1-3,5,6]. Diagnosis is performed through immunological tests of the blood and cerebrospinal fluid as well as imaging exams, such as computerized tomography (CT) and magnetic resonance (MR) [1,5,7]. Correlating clinical, radiological and immunological aspects, Del Bruto [8] has proposed absolute, major, minor and epidemiological criteria that allow both the probable and definitive diagnosis of NCC. Few publications report psychiatric disorders associated with NCC. The most commonly reported manifestations are impaired consciousness and a decline in cognitive functions [2,5]. This paper describes the case of a patient with racemose NCC and psychiatric symptoms. A discussion is also offered on neuroimaging findings of this uncommon form of presentation.
Case Report
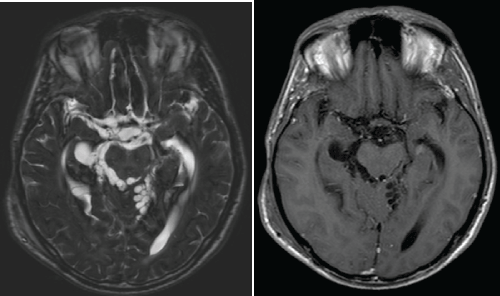
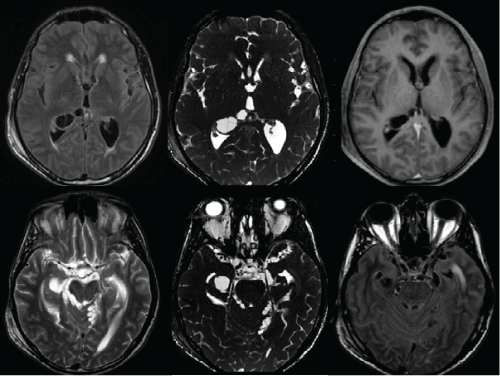
A previously healthy 39-year-old single male sought urgent care at the hospital of the State University of Campinas (Brazil) with a two-month history of disorientation characterized by incoherent speech, difficulty organizing his thoughts, forgetfulness and crying. The patient reported episodes of fainting, headache, blurred vision and dizziness. The blood exam upon admission demonstrated leukocytosis (18.000/mm3 at the cost of segmented neutrophils (87.4%)). The spinal fluid revealed discrete pleocytosis (20 cells/mm3), with a predominance of lymphocytes (58%), the presence of plasmocytes (38%) and eosinophils (1%) as well as normal protein and glucose concentrations. Immunological reactions using ligase chain reaction and the study of bacteria and fungi as well as serological tests for human immunodeficiency virus, hepatitis, cytomegalovirus and syphilis were all negative. CT and MRI were performed and the images revealed multiple cysts in the subarachnoid spaces, basal cisterns as well as the infratentorial and supratentorial ventricular system, together with hydrocephalus and cerebral fluid transudation. The findings were compatible with racemose NCC (Figures 1 and 2). The patient was submitted to urgent ventriculoperitoneal shunting and treated with albendazole for 28 days. A second CT scan (23 days after the first) demonstrated regression of the lesions (Figures 3 and 4). Moreover, complete resolution of the psychiatric symptoms occurred.
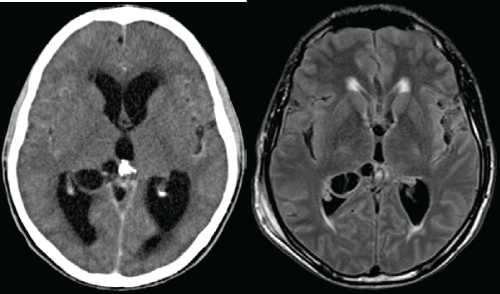
Figure 1: Axial images in the axial plane of the anterior and posterior of the lateral ventricles and third ventricle, compatible with NCC racemosa horns.
1a. Post- contrast CT; cystic images with parietal enhancement in the posterior horn of the right lateral ventricle (VLD). Hydrocephalus and hipodensidades in periventricular white matter, cerebrospinal fluid compatible with transduction.
1b. MRI FLAIR sequence; isointensos the CSF cysts with hyperintense wall inside the VLD. Foci of periventricular compatible with hyperintense cerebrospinal fluid transudation.
Discussion
NCC is endemic in the majority of developing countries and is transmitted through the ingestion of water and food contaminated with the larval form of Taenia solium. Pigs are the intermediate host; eggs are transmitted to pigs through human feces that contain the parasite [1-3]. Despite being the most common parasitic infection of the central nervous system, an unusual case of NCC (the racemose form) is reported herein, with an uncommon clinical presentation characterized predominantly by psychiatric symptoms with a sub-acute progression. NCC affects males and females and all age groups equally. This polymorphic disease has a variety of completely nonspecific signs and symptoms. The clinical variability and unpredictability are closely related to the inconstant behavior of the parasite in the face of the diversified immune response in the host. The extremes of its clinical presentation range from asymptomatic patients to catastrophic or even fatal progression. Epilepsy and headache are the most common manifestations of NCC [1-3,5]. Psychiatric aspects range from a poor intellectual performance to dementia [2,5,9]. Psychotic episodes have been described, such as disorientation, paranoid ideation, psychomotor agitation, violent behavior and visual hallucinations. Prior to the advent of CT, many patients were hospitalized in psychiatric institutions for years with no diagnosis of the organic disease [1,2]. Analyzing 123 patients with NCC, Levav et al. [10] found behavioral dysfunctions related to inhibitory control, motor control and visualmotor integration. According to the authors, NCC compromises the impulse control of motor actions (orbital-frontal gyrus). Estimates of the prevalence of mental alterations in NCC are variable and depend on the sample of patients studied as well as the method used for the diagnosis of the psychiatric disorder. Psychiatric manifestations are generally described in combination with intracranial hypertension and epilepsy and rarely manifest in an isolated fashion. In general, the psychiatric population has a fivefold greater incidence of NCC in comparison to the general population. [4,9,11]. Forlenza et al. [9,11] used a standard psychiatric assessment tool and followed up 38 patients with NCC, among whom 75% exhibited psychiatric manifestations and 87.5% exhibited cognitive decline. Depression was the most common psychiatric diagnosis (52.6%) and 14.2% of patients exhibited psychotic symptoms. Another study also found an association between NCC and depression; the authors report that the incidence of depression in the patients evaluated was higher than that found in the generally population [12]. Capitão et al. [13] investigated psychological aspects characterized by a failure to comprehend reality, spatial disorientation, time confusion, low control of aggressive impulses and the development of psychosis with delirium and hallucinations. In the patient described herein, the symptoms were predominantly in the psychiatric realm. As the patient also complained of headache and dizziness, the decision was made to investigate an organic cause for the psychiatric symptoms. The neuroimaging exams revealed the uncommon racemose form of NCC, which is generally related to symptoms of intracranial hypertension, such as vomiting and papilledema [1,2]. However, the patient did not exhibit these symptoms.
The cellulosae form is characterized by cysts with scolex and intraparenchymatous or ventricular localization. In the racemose form, large translucent, multi-lobed vesicles without scolex are seen in the interior of the subarachnoid spaces [14]. The imaging findings (RM or TC) depend on the location and development phase of the cysticerci (vesicular, colloidal, granular nodular and calcified nodular) [6,15- 17]. It should be pointed out that the same patient can exhibit lesions in different stages of the disease simultaneously [1,6,7,16]. NCC is classified as parenchymatous, intraventricular, cisternal-subarachnoid or spinal, depending on the location [6,7,16]. The ventricular location is the second most common, especially the fourth ventricle [6]. The intensity of the signal from the intraventricular cyst is discretely higher than that of the cerebral fluid. Thus, dilation of the ventricular system is commonly detected and is likely related to the obstruction of the flow of the cerebral fluid [6,15,17,18]. Aqueduct stenosis and epididymitis may also occur [5]. NCC in the subarachnoid space commonly involves basal cisterns and sylvian fissures. With MR, the cysts have a signal similar to that of the cerebral fluid and are not highlighted by the intravenous contrast. There is a mass effect, leading to an increase in the local subarachnoid space and a multi-loculated appearance. The scolex is generally not seen. There may also be discrete leptomeningeal highlighting [5,6,15]. The clinical suspicion of NCC and prompt treatment are fundamental to a good prognosis, as occurred in the case described herein. The successful control of cysticercosis depends on the adoption of measures directed as the prevention of the taeniasis/ cysticercosis complex in a simultaneous, integrated fashion to avoid the occurrence of severe cases, such as the present one.
Conclusion
Rapid diagnosis and prompt treatment of this uncommon form of NCC allowed the complete resolution of the psychiatric symptoms and regression of the lesions. These findings demonstrate the decisive role of neuroradiology in such cases.
Author Contibutions
We have conceived, designed and written the case report.
References
- Del-Brutto OH (2012) Neurocysticercosis: A Review. The Scientific World Journal. 2012: 1-8.
- Sotelo J, Del Brutto OH (2000) Brain cysticercosis. Arch Med Res 31: 3-14.
- Takayanagui OM (2013) Neurocysticercosis. ArqNeuropsiquiatr 71: 710-713.
- Agapejev S (2003) [Clinical and epidemiological aspects of neurocysticercosis in Brazil: a critical approach]. ArqNeuropsiquiatr 61: 822-828.
- Litt AW, Mohuchy T (1999) Case 10: neurocysticercosis. Radiology 211: 472-476.
- Lucato LT, Guedes MS, Sato JR, Bacheschi LA, Machado LR, et al. (2007) The role of conventional MR imaging sequences in the evaluation of neurocysticercosis: impact on characterization of the scolex and lesion burden. AJNR Am J Neuroradiol 28: 1501-1504.
- Kimura-Hayama ET, Higuera JA, Corona-Cedillo R, Chávez-Macías L, Perochena A, et al. (2010) Neurocysticercosis: radiologic-pathologic correlation. Radiographics 30: 1705-1719.
- Del Brutto OH, Wadia NH, Dumas M, Cruz M, Tsang VC, et al. (1996) Proposal of diagnostic criteria for human cysticercosis and neurocysticercosis. J NeurolSci 142: 1-6.
- Forlenza OV, Filho AH, Nobrega JP, dos Ramos Machado L, de Barros NG, et al. (1997) Psychiatric manifestations of neurocysticercosis: a study of 38 patients from a neurology clinic in Brazil. J NeurolNeurosurg Psychiatry 62: 612-616.
- Levav M, Mirsky AF, Cruz ME, Cruz I (1995) Neurocysticercosis and performance on neuropsychologic tests: a family study in Ecuador. Am J Trop Med Hyg 53: 552-557.
- Forlenza OV, Vieira Filho AH, Machado Ldos R, Nóbrega JP, de Barros NG (1998) [Depressive disorders associated with neurocysticercosis: prevalence and clinical correlations].ArqNeuropsiquiatr 56: 45-52.
- Almeida SM, Gurjão SA (2010) Frequency of depression among patients with neurocysticercosis.ArqNeuropsiquiatr 68: 76-80.
- Capitão CG, Barra LAC, Bedaque EA, Martinelli FLB (2008) Neurocysticercosis: neurologic and psychological aspects. Rev PanamInfectol 10(1):30-38.
- Singh S, Gibikote SV, Shyamkumar NK (2003) Isolated fourth ventricular cysticercus cyst: MR imaging in 4 cases with short literature review. Neurol India 51: 394-396.
- García HH, Del Brutto OH (2003) Imaging findings in neurocysticercosis.Acta Trop 87: 71-78.
- Noujaim SE, Rossi MD, Rao SK, Cacciarelli AA, Mendonca RA, et al. (1999) CT and MR imaging of neurocysticercosis. AJR Am J Roentgenol 173: 1485-1490.
- Yeaney GA, Kolar BS, Silberstein HJ, Wang HZ (2010) Case 163: solitary neurocysticercosis. Radiology 257: 581-585.
- Kelesidis T, Tsiodras S (2011) Extraparenchymalneurocysticercosis in the United States: a case report. J Med Case Rep 5: 359.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 15816
- [From(publication date):
February-2015 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 11204
- PDF downloads : 4612