Review Article Open Access
Different Radiographic Modalities Used for Detection of Common Periodontal and Periapical Lesions Encountered in Routine Dental Practice
Vandana Kumar*, Kirandeep Arora and Hema Udupa
School of Dentistry, Oral and Maxillofacial Radiology, Kansas City, USA
- *Corresponding Author:
- Vandana Kumar
school of Dentistry
Oral and Maxillofacial Radiology
650E, 25th street Kansas City
Missouri 64108, USA
Tel: 816 235-2664
E-mail: kumarva@umkc.edu
Received Date: June 23, 2014; Accepted Date: September 17, 2014; Published Date: September 23, 2014
Citation: Kumar V, et al. (2014) Different Radiographic Modalities Used for Detection of Common Periodontal and Periapical Lesions Encountered in Routine Dental Practice. J Oral Hyg Health 2:163. doi:10.4172/2332-0702.1000163
Copyright: © 2014 Kumar V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
The objective of this article is to review the literature which describes the different radiographic modalities used for detection of osseous defects due to periodontal and periapical disease. Despite inherent limitations associated with conventional two-dimensional (2D) intra- and extra-oral radiographs, these continue as the mainstay for assessments of periodontal and periapical defects. Three dimensional CBCT scans are considered as a useful complement to these conventional radiographic techniques. This article gives an overview of common periodontal and periapical lesions encountered in routine clinical practice and various radiographic modalities used for their detection.
Keywords
Periodontal defects; Bony pockets; Furcation involvement; Periapical and Bitewing radiographs; Cone Beam CT; Periapical lesions; Periapical sclerosing osteitis
Introduction
Periodontium consist of cementum, periodontal ligament and alveolar bone. The term periodontitis/periodontal disease represent a group of disease that affects the surrounding and supporting tissues of teeth. Periodontal disease can be broadly classified as gingival diseases (gingivitis) and periodontitis. Gingivitis presents as inflammation of the soft tissue surrounding the teeth and is characterized by gingival swelling, and erythema. Periodontitis is an inflammatory destruction of the supporting apparatus of the teeth, including cementum, periodontal ligament and alveolar bone which results in gradual loosening of teeth. Although periodontitis is always preceded by gingivitis, gingivitis does not always progress to periodontitis.
Bacterial plaque is the chief causative factor for periodontal disease and apical migration of this bacterial plaque causes bone destruction leading to osseous defects. Other factors like stress, occlusal trauma, smoking, hypertensionand diabetes also contribute to greater risk of periodontal disease [1]. The formation of osseous defect is either related to occlusal stress on the tooth or to original anatomy of the alveolar process [2]. In recent research, a strong correlation is found between periodontal disease and cardiovascular disease [3]. It is found that bacterial microorganisms that cause periodontitis travel through the blood stream and have high affinity for the development of atherosclerotic plaque, notably involving the cardiac and carotid endothelium, leading to coronary heart disease and vice versa [4].
The pulp cavity is the central part of the tooth that extends into the root as root canal which opens into the periodontium via apical foramen and is enclosed all around by dentin. Healthy periapical tissues exhibit following important features:
1. Periodontal ligament space (PDL) : A thin, continuous radiolucent line around the outline of the root
2. Lamina dura :A thin, continuous radiopaque line adjacent to the radiolucent line
3. The trabecular pattern and density of the surrounding cancellous bone
Any changes in the thickness, continuity, density of these features may suggest the presence of pulpal, periodontal, and various pathologic disorders. Advancing pulpal inflammation when exits the apical foramen will exhibit radiographic signs such as widened PDL and poorly demarcated periapical low density area due to demineralization and these changes are typically located at the apex of the tooth. .Sometimes these lesions extend along the lateral surface of root due to the presence of the accessory canals. Widening of PDL is an early sign of periapical inflammation [5-7]. The prevalence of apical periodontitis associated with root-filled teeth was reported to be as high as 64.5% in a cross sectional study of populations [8-10]. Early detection of periodontal and periapical disease and correct assessment of the bone condition is essential for the diagnosis, treatment planning and prognosis of periodontal disease [7,11].
Current approaches to diagnose periodontal disease include probing of gingival tissues and radiographs to evaluate osseous support and periapical pathosis. Due to lack of stable reference point and standardization and calibration of periodontal probe reading, it is not considered a reliable method for evaluation of advanced periodontal disease. Radiographs provide an overview of the amount of bone present and serve as a permanent record for future comparison to assess bone loss/ gain. Radiographs are also used effectively in patients having periapical lesions to determine the extent and severity of the disease.
In the following sections, common periodontal and periapical osseous defects encountered in routine clinical practice would be elaborated and various diagnostic imaging methods along with their associated strengths and limitations would be discussed.
Common radiographic modalities for detection of periodontal and periapical lesion
The success of periodontal therapy depends on many factors. One of the most important factors is an accurate image of morphology of periodontal bone destruction that would influence the treatment modality and eventually the outcome of the periodontal therapy. Intraand extra-oral imaging modalities are available to display periodontal structures. The extraoral panoramic radiograph can be utilized as an alternative assessment. Though it provides means of viewing larger area and can be used in assessing periapical lesions like condensing osteitis, florid osseous dysplasiaetc. but has very little diagnostic value in assessing alveolar bone levels [12]. Patient positioning error and superimposition of ghost images often result in suboptimal projections and limit comparisons with follow-up images. Superimposition and distortion of structures, blurring of anatomical landmark and loss of detail are the inherent limitations of panoramic radiograph that reduce their value in evaluation of osseous defects due to periodontal or periapical disease [13]. Most common two dimensional (2D) intra oral radiographs used to determine osseous defects are bitewings and periapical radiographs, with the paralleling extension cone method. These are easy to acquire, are cheap and have high resolution details [14]. Bitewings present the most favorable imaging geometry for periodontal bone level assessment; best detection performance is achieved with horizontal angulation perpendicular to the tooth surfaces, and vertical angulation with a positive or negative tilt of 12-15 degrees relative to the perpendicular [15]. Vertical bitewings are used where there is bone loss > 4 mm [16]. The disadvantage of bitewings is that apices of the teeth are not visible; therefore, one cannot estimate percentage of bone loss that has taken place [17]. Full mouth periapical radiographs are also used to diagnose osseous defects and are found to be more effective in posterior segment in mandible than in maxilla due to denser bone in mandible [12]. The disadvantages of full mouth periapical radiographs are, that they are time consuming, require multiple films and have low patient tolerance [18]. In comparison to bitewing radiographs, periapical radiographs also present more geometric distortion [16]. Intraoral digital radiographic imaging offers the clinician an improved way for periodontal diagnosis and treatment planning. It not only reduces radiation exposure, [19-22] but also optimizes assessment of oral structures, improving the accuracy of periodontal diagnosis [23]. However, these 2D intraoral radiographic methods are limited by overlapping anatomical structures [24,25] difficulty in standardization [26,27] and by underestimating the size and occurrence of bone defects [25]. Funnel-shaped or lingually located defects are difficult to detect in these radiographs [28] and destruction of the buccal plate can be undiagnosed or undistinguished from lingual defects [29]. Studies have shown that bone loss can be underestimated by 1.5 mm, with large variations between examiners with these modalities [30].
For the long term assessment of periapical disease, periapical radiographs play a vital role in preoperative, post-operative and follow up appointments. Radiographic signs of apical periodontitis include radiolucent changes in periradicular trabecular pattern and changed shape and width of the periodontal ligament (PDL). However, small periapical lesions < 1 to 2 mm go undetected on periapical radiographs and the radiographic appearance of periapical lesions is always smaller than the histologic extent of the lesion [31,32].
To address these issues, Cone beam computed tomography has been explored because it enables cross-sectional and three dimensional analyses without distortion similar to multi-slice conventional tomography (CT) however, it does so with reduced acquisition times, lower effective radiation doses, and decreased financial burdens when compared with CT [33,34]. Introduction of CBCT technology presents the opportunity for 3D assessment of dental and craniofacial anatomy without the inherent limitations of conventional 2D imaging [35]. That is, an assessment can be conducted in all three planes of space without image distortion, superimposition of structures, and differential magnification of the image based on geometry. Research comparing the use of three-dimensional (3D) volumetric images and 2D images in artificial bone defects has shown that CBCT has sensitivity of 80-100% in the detection and classification of bone defects, while intra-oral radiographs present a sensitivity of 63-67% [27,36-38]. CBCT images are well-known to provide detailed anatomy of the teeth and bones as well as allow for evaluation of the periapical lesions in multiple planes and aids in improved detection of the disease [39]. CBCT has a role in the identification of root canal systems, notably for the identification of presence or absence of a second mesiobuccal canal (MB2) in maxillary first molars which are not visible on periapical radiographs [40,41].
Although, CBCT is able to readily detect simulated defects, they lack clinical applicability because of failure to use an appropriate reference standard to explain the true presence of disease. Crosssectional imaging does offer a potential means of resolving resorption (internal or external) and perforations, as literature shows that CBCT may be useful in this respect with improved sensitivity. A question has to be asked, however, whether this will have a significant impact on management of the patient. In the case of perforations by posts, due regard has to be given to degradation of images by beam hardening artifact arising from metal post and obturation material like gutta percha, which may mask features in the roots and surrounding bone [5,6,42]. Further research is needed addressing the impact on management decisions and, for now, it seems logical to consider CBCT only when conventional radiography has been tried and failed to answer the question and when a significant treatment decision (e.g. to extract or not) has to be made [43]. The literature shows that a request for CBCT is justified for the periodontal surgical planning of patients with severe periodontal diseases such as aggressive periodontitis, for regenerative or mucogingival surgical planning and for planning of implant placements. These surgical procedures are costly, difficult to plan and need precise diagnosis [14]. Periapical radiographs result in lower radiation doses to the patient and are less costly, hence should be indicated for simpler cases.
The available intra-oral and extra-oral 2D and 3D radiographic modalities are invaluable diagnostic tool that can be used effectively in a wide variety of clinical and research situations. However, like any other diagnostic procedure involving ionizing radiation, their use should involve clinical judgment rather than routine practice. Recent studies have indicated that medical radiation, most notably computed tomography (CT), now accounts for more radiation exposure to the U.S. population than background radiation [44,45]. Although CT typically represent less than 11% of all imaging performed at most universitybased practices, diagnostic CT can account for as much as 70% of the overall radiation dose generated in radiology departments [46]. The doses from CBCT are significantly lower than conventional CT, yet are higher than doses from the traditional views used in dentistry [47-49]. Significant differences in dose for the same examination have been reported for different CBCT units and significant differences in dose have been reported for different fields of view (FOVs) or techniques with the same unit [50-53]. In a study by Roberts et al, the i-CAT CBCT scanner was investigated for various imaging protocols commonly used in clinical practice [52]. The effective doses, based on 2007 (E2007) ICRP guidelines, were 206.2 μSv for full FOV of the head; 133.9 μSv for a 13 cm scan of the jaw; 188.5 μSv for a 6 cm highresolution scan of the mandible; 93.3 μSv for a 6 cm high-resolution scan of the maxilla; 96.2 μSv for a 6 cm standard scan of the mandible; and 58.9 μSv for a 6 cm standard scan of the maxilla [54]. When eight different dentoalveolar and maxillofacial CBCT units and a 64-slice multi-detector computed tomography (MDCT) unit were compared for radiation according to E2007, exposures for large FOV CBCT units ranged from 68 to 1,073 μSv and for medium FOV CBCT units ranged from 69 to 560 μSv, whereas for the MDCT unit with a similar FOV, the exposure was 860 μSv [55]. In a study by Ludlow JB et. al, effective radiation dosage associated with 2D radiographic modalities based on E2007 were enumerated as follows [49]:
a) 34.9 μSv for full mouth radiographs (FMX) with photo-stimulable phosphor (PSP) storage or F-speed film with rectangular collimation
b) 5.0 μSv for four-image posterior bitewings with PSP or F-speed film with rectangular collimation was ;
c) 14.2 μSv for panoramic Orthophos XG (Sirona Group, Bensheim, Germany) with charge-coupled device (CCD),
d) 24.3 μSv for panoramic ProMax (Planmeca, Helsinki, Finland) with CCD.
These dosages were far less when compared to effective radiation dosage associated with CBCT/MDCT. Therefore, attention to radiation hygiene by following the fundamental principle of choosing exposures “As Low As Reasonably Achievable” (ALARA) for diagnostic radiology is imperative. CBCT procedures must be reserved for selected cases— and appropriately collimated down to the chosen region of interest.
Osseous defects as result of periodontal disease
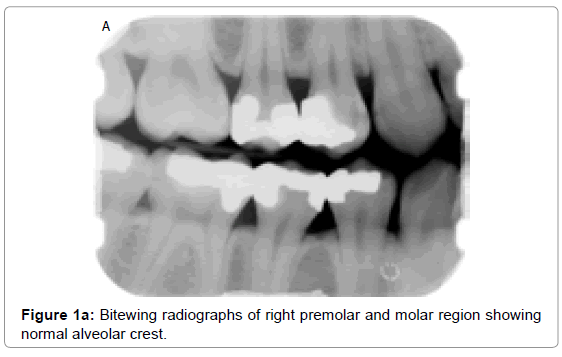
Normal alveolar bone supporting dentition has a characteristic radiographic appearance. It exhibits a thin opaque cortical bone that covers the alveolar crest. The height of crest lies at a level approximately 0.5 to 2.0 mm below the level of cementoenamel junction (CEJs) and is continuous with lamina dura of adjacent teeth (Figure 1a and 1b). Care must be taken in using CEJ as a reference point in case of over erupted and severely attrited teeth.
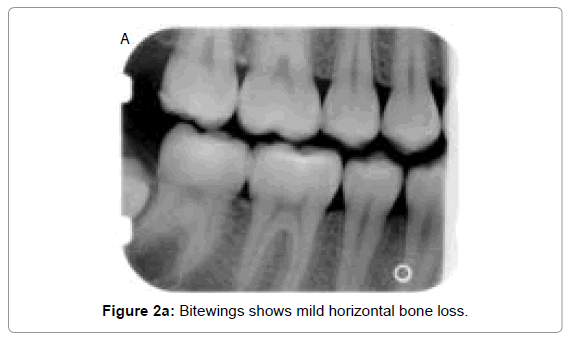
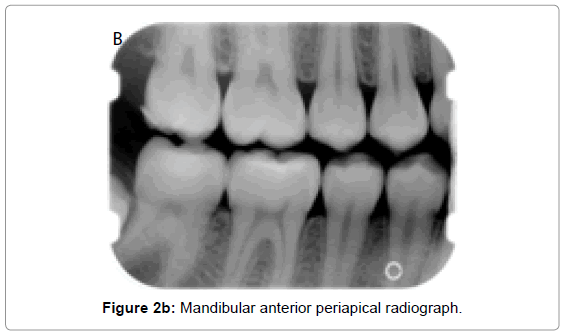
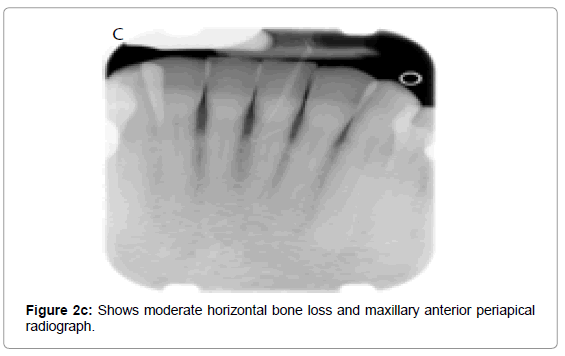
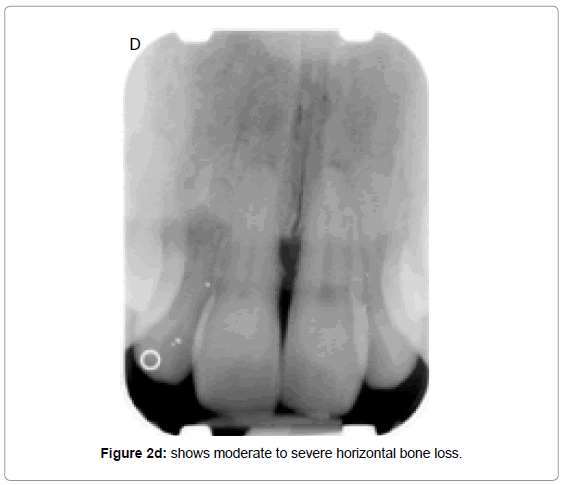
Osseous defects as a result of periodontal disease is classified clinically into horizontal (even) and angular (vertical) defects. In horizontal bone loss, the height of alveolar bone is symmetrical and parallel to an imaginary line joining CEJ of adjacent teeth. There occurs resorption of buccal, lingual cortical walls including the interdental bone. It can be categorized as mild, moderate or severe, depending on its extent (Figures 2a, b, c and d).
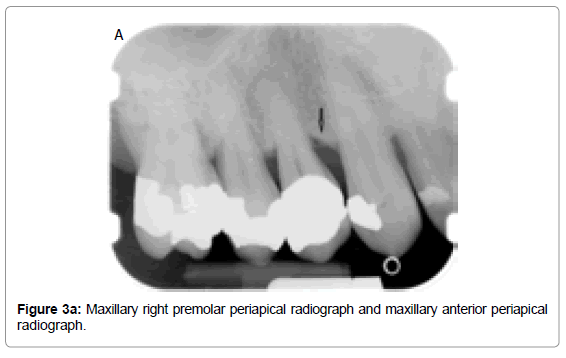
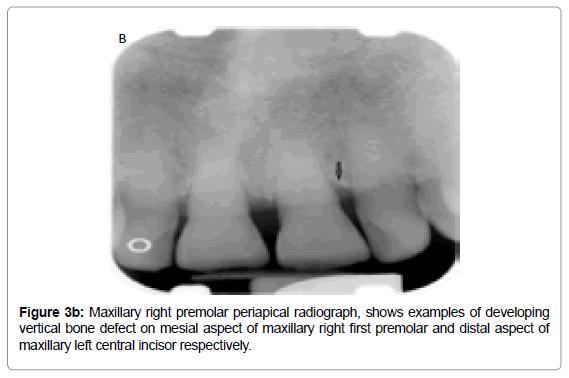
In the vertical or angular osseous destruction, the bone loss is unsymmetrical; alveolar crest is not parallel to the level connecting the CEJ of the adjacent teeth (Figure 3a). These defects develop when bone loss progresses down the root of the tooth, resulting in deepening of the clinical periodontal pocket. The early vertical defects appear as abnormal widening of the PDL space at alveolar crest (Figure 3b). Further vertical osseous destruction leads to the formation of osseous defects where the base of the defect is located apically to the alveolar crest [56,57].
Different classifications of bone defects have been proposed. Goldman & Cohen (1958) described the morphology of various bone defects and classified them according to the number of osseous walls present [58]. Glickman (1964) presented a specific description of bone deformities produced by periodontal disease, classifying bone defects as osseous craters, infrabony defects, bulbous bone contours, hemisepta, inconsistent margins and ledges [57]. Prichard (1967) expanded this classification by including furcation involvement and indicated that resorptive lesions may also be complicated by anatomic aberrations of the alveolar process, i.e., thick marginal ledges, exostosis and tori. Additional anatomic aberrations of the alveolar process are isolated areas in which the root is denuded of bone to a varying extent (dehiscence and fenestrations) [59]. Other classifications were introduced later and represented the combinations of the existing descriptions.
Based on the classifications proposed, morphology of bone defects can be described as follows [56]:
1. Interdental crater/ two wall bony defect is a saucer shape concavity in the interdental bone confined within facial and lingual walls. These are the most common osseous defects and are most commonly found in the posterior segment of the mandible.
2. Three- wall bony defect has bony walls on three sides and tooth root forming the fourth wall
3. Four- wall defect is a circumferential defect that completely surrounds the root of the tooth.
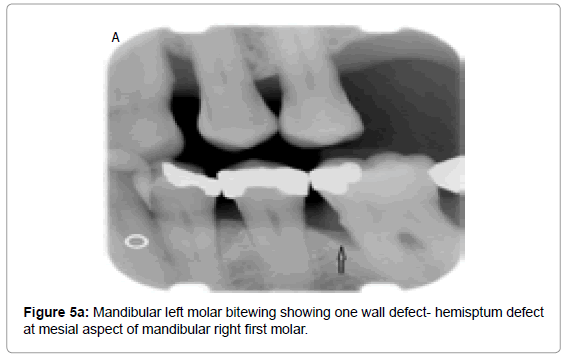
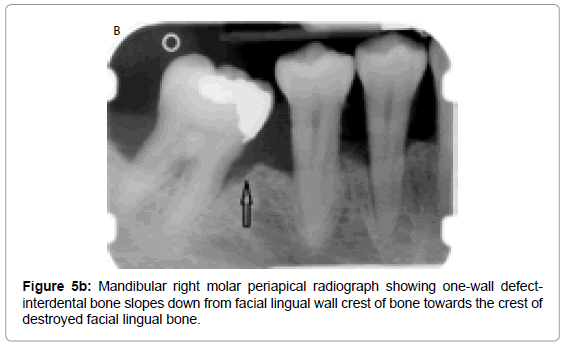
4. Hemiseptum defect/ One-wall defect is where one bony wall of the interseptal bone remains after the mesial and distal portions of the interseptal bone has been destroyed. It is identical to vertical or angular deformities.
5. Furcation involvement: extension of bone loss between roots of mutirooted teeth, eliminating the bone covering the root [60]. This is further subcategorized as:
Grade 1: Incipient bone loss, radiographic changes are not usually seen as bone loss is minimal
Grade 2: There is destruction of bone in one or more aspect of furcation, but part of alveolar bone and periodontium remains intact to allow partial penetration of the probe. These too may or may not be seen on traditional radiographs as they get obscured due to overlapping of roots, angulation of x-rays or due to thick inter- radicular bone.
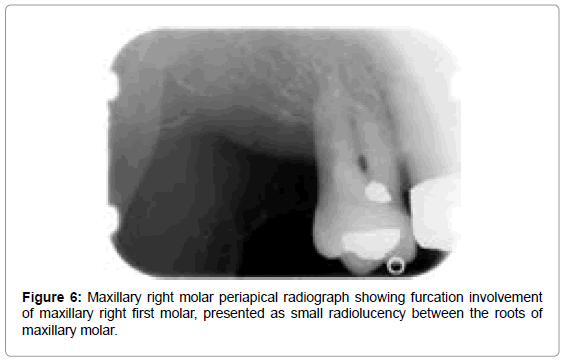
Grade 3: Inter radicular bone is completely absent allowing probe to penetrate completely. Traditional radiographs reflect this defect as a small radiolucency between roots. Grade 3 furcations in maxillary posterior teeth are difficult to diagnose due to overlapping of roots
Grade 4: Similar to grade 3 but gingival tissue is recessed and is detected clinically and radiographically
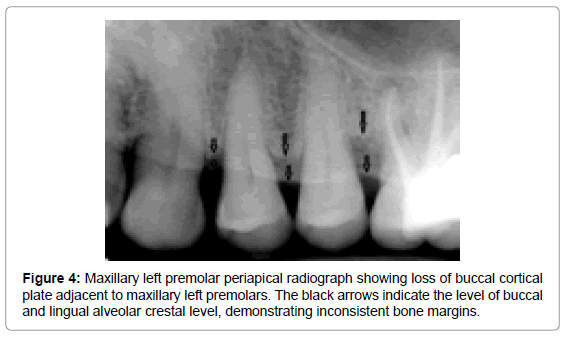
The vertical bone defects, especially three and four wall defects, are difficult to detect on a conventional radiograph because buccal/ lingual cortical plates remain superimposed over the defect. Clinical and surgical evaluation of these defects is the best mode of determining the number of the remaining walls. Two wall and one wall defects can be identified on conventional radiographs. Radiographically, interdental craters / two wall defects can be identified as band like regions or inconsistent bone margins (Figure 4), whereas one-wall defect presents as ramp like appearance, because the inter-dental septal bone slopes down from the facial/ lingual wall crest of bone towards the crest of the destroyed facial/ lingual bone (Figure 5a and 5b). Grade 3 and grade 4 furcation involvement of mutirooted teeth can also be revealed on conventional radiographs as radiolucency between roots (Figure 6).
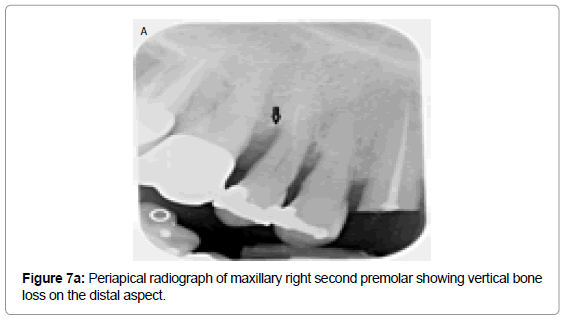
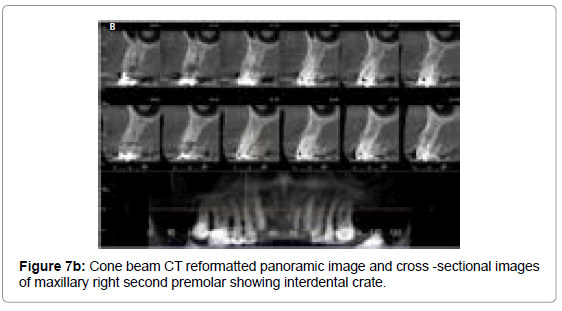
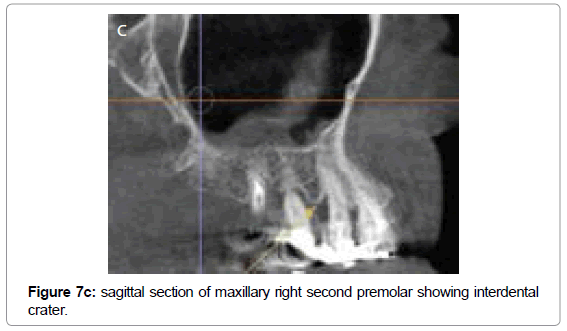
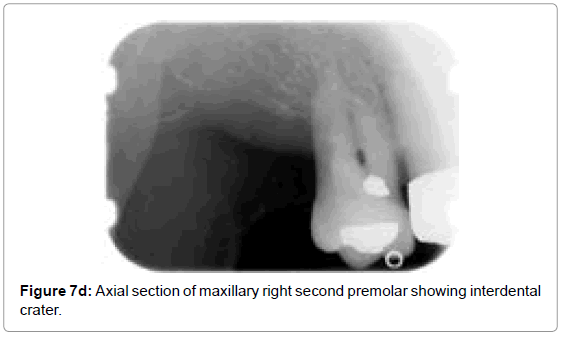
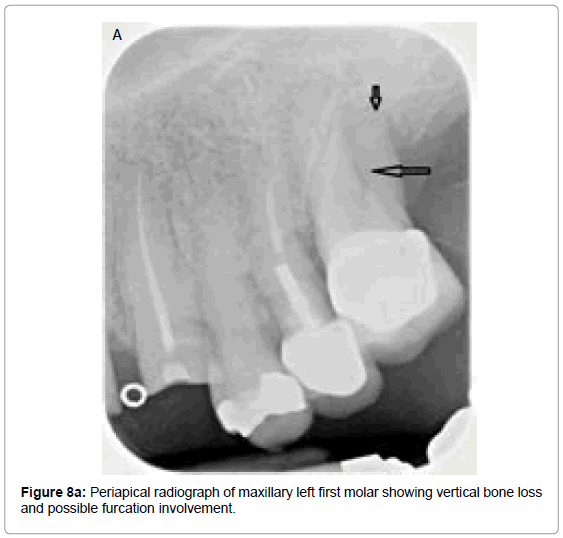
Vandenberghe et al. observed that the cross-sectional slices from CBCT data allows better assessment of periodontalbone levels with an average underestimation of 0.29 mm compared with 0.56 mm in periapical digital radiographs [38]. Periapical radiograph of the maxillary right second premolar (Figure7a) exhibits distal vertical bone loss suggesting interdental crater, whereas CBCT reformatted panoramic image and cross-sectional images of maxillary right second premolar (Figure7b) and associated sagittal (Figure 7c) and axial sections (Figure 7d) clearly exhibits loss of facial and distal walls. The accuracy of CBCT to diagnose molar furcations has been identified. CBCT generated data adds substantial amount of information about the form of the furcation and severity of the lesions that cannot be obtained from the conventional radiographs or clinical assessments [61,62]. In another radiographic example presented here, periapical radiograph of maxillary left first molar (Figure 8a) shows vertical bone loss on its distal aspect and possible furcation involvement. CBCT reformatted panoramic image and cross-sectional images (Figure 8b) of the same tooth shows clearly the furcation involvement, periapical radiolucencies and severe bone loss all around it. These defects are very difficult to detect on conventional radiographs.
Osseous defects as result of periapical disease
Osseous destruction as a result of periapical disease could be classified broadly as of inflammatory and non-inflammatory origin. Inflammatory periapical lesions can produce osseous changes around the apex of a tooth as a result of either pulpal necrosis or due to extensive periodontal disease causing destruction of the periapical tissues. Periapical lesions causing osseous defects present radiographically as radio-lucency, opacity or a combination of both around the root of the tooth. These are often incidental findings during routine dental imaging studies, or may be seen as manifestations of other diseases of odontogenic and non odontogenic origin, including cysts and neoplasms. Radiolucent or low density presentations are categorized as periapical rarefying osteitis, including periapical abscess, granuloma, and cyst/ tumor while the radiopaque presentations are categorized as periapical sclerosing osteitis and idiopathic osteosclerosis.
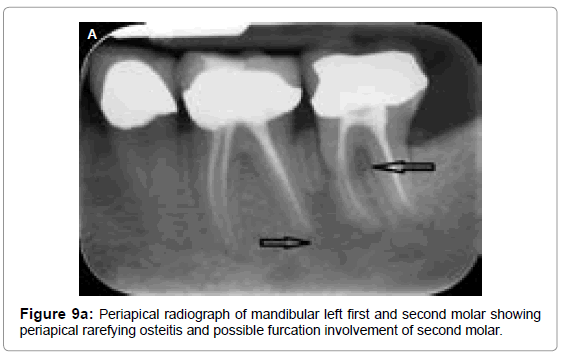
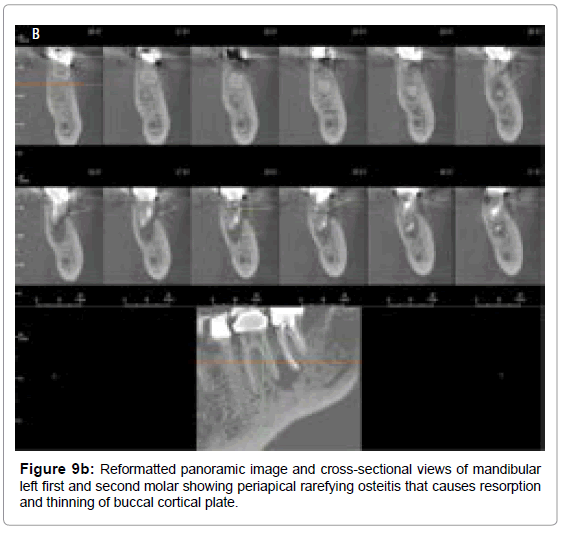
Periapical rarefying osteitis occurs as a result of bone resorption in the periapical areas surrounded by a sclerotic periphery. Early lesions presents as a widening of the PDL space followed by a gradual loss of apical lamina dura. As the lesion grows with resorption and thinning of associated buccal and lingual cortices and possible expansion of the region. Periapical radiograph of root canal treated mandibular left first and second molar (Figure 9a) shows periapical rarefying osteitis associated with its distal root that extends up to the mesial root of adjacent mandibular left second molar, involving the interdental bone between them. The radiograph also suggests the furcation involvement of mandibular left second molar. Reformatted panoramic images and cross-sectional views of same teeth (Figure 9b) shows the periapical rarefying osteitis causing resorption and thinning of buccal cortical plate on distal aspect of mandibular first molar and clearly exhibits furcation involvement of mandibular left first and second molars.
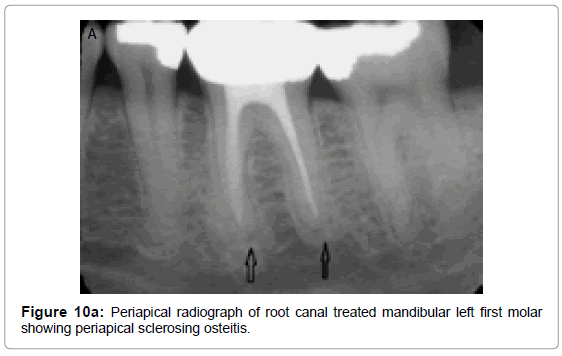
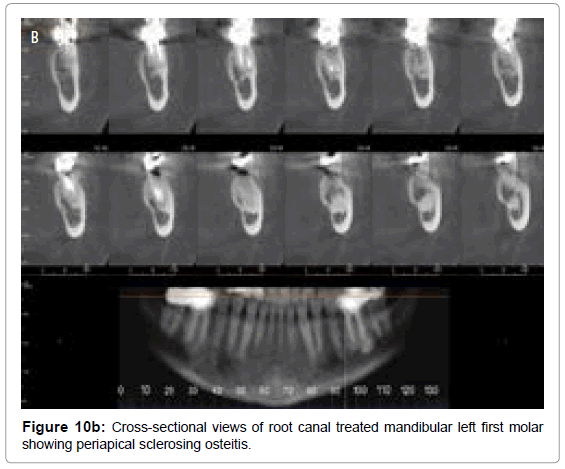
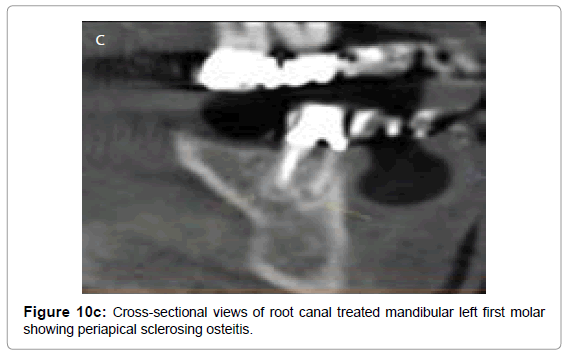
Periapical sclerosing osteitisalso known as condensing osteitis or focal sclerosing osteitis occurs as a result of chronic periodontal and endodontic infections in a tooth. Individual thickening of the trabeculae is noted within the marrow spaces surrounding the roots of the affected teeth with sclerosis of periapical bone. This is a result of surrounding bone attempting to wall off the inflammation or repair the bone affected by the inflammatory process. Radiographically, condensing osteitis appears as a uniformly dense radiopaque mass adjacent to the apex of the tooth with well-defined margins combined with loss of apical lamina dura and widening of the PDL. Periapical radiograph (Figure 10a) and reformatted images and cross-sectional views (Figure 10b) and sagittal section (Figure 10c) of root canal treated mandibular left first molar demonstrates periapical sclerosing osteitis involving apices of mesial and distal roots.
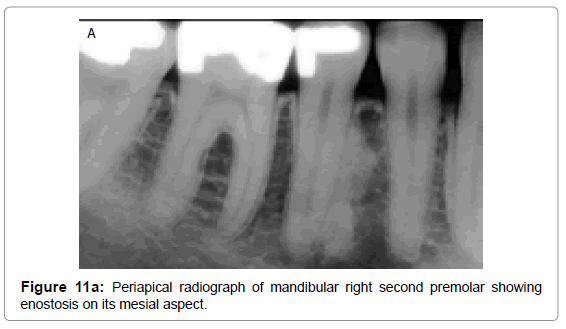
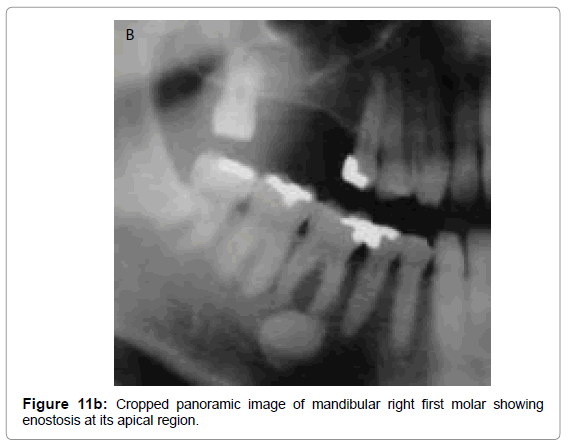
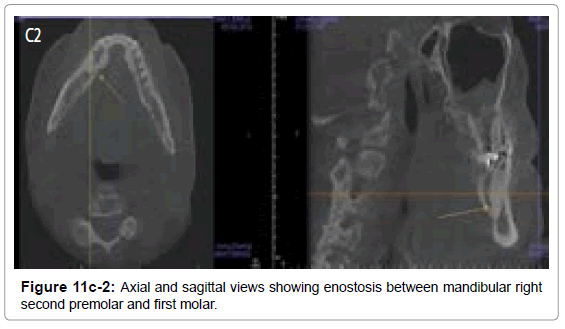
Idiopathic osteosclerosis or dense bone island or enostosis are localized areas of increased radiopacities that occur due to unknown etiology. They occur in the periapical areas, extend beyond the apices of associated teeth and can also be found in the edentulous areas. Radiographically, these present as well-defined, densely homogeneous, non expansile radiopacity with normal PDL space and lamina dura when in close proximity to the apex of a tooth. (Figures 11a,11b,11c-1 and 11c-2). They are asymptomatic and are found incidentally during routine dental imaging.
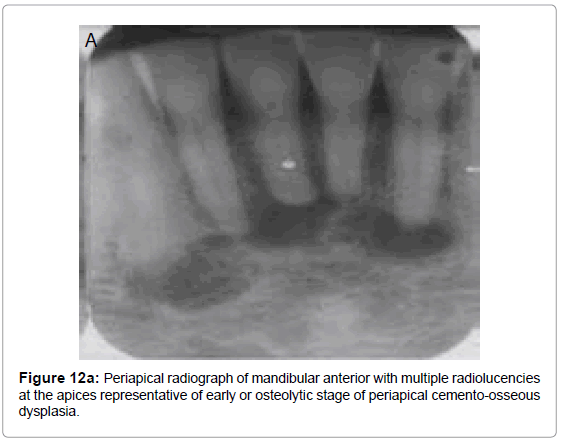
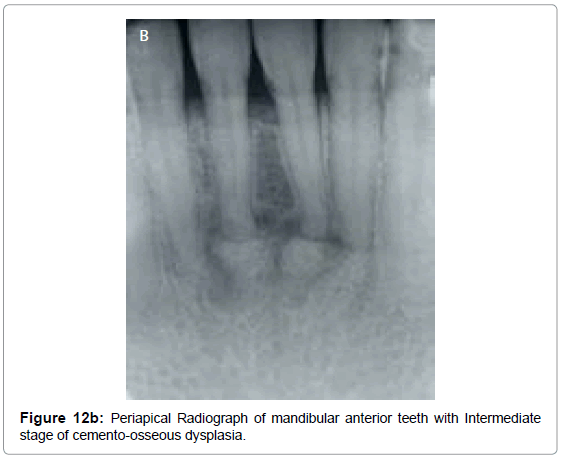
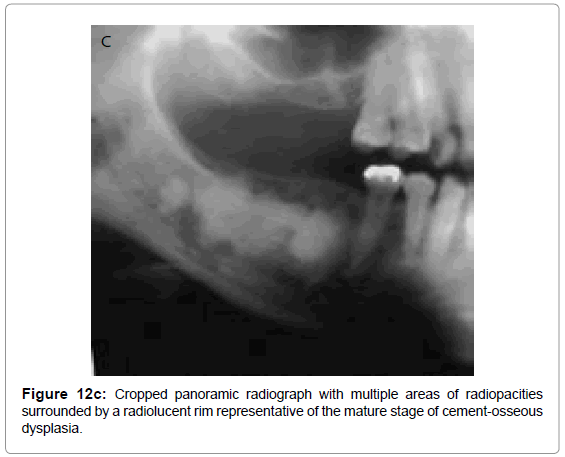
Non-inflammatory periapical lesion are a group of non-neoplastic lesions collectively called as “benign fibro osseous lesions”. Normal bone is replaced by fibrous connective tissue containing abnormal cementum or bone. Osseous dysplasia (OD) or cemento-osseous dysplasia (COD) is an example of fibro-osseous disease that occurs commonly in jaws. These lesions are confined to dentulous or edentulous portions of the jaws. In 2005, WHO described three clinical presentations of OD/ COD : periapical OD/COD, focal OD/COD and florid OD/COD. Radiographically, these lesions exhibit osteolytic, intermediate and mature stages. The osteolytic stage appears as welldefined radiolucencies at the apices of associated teeth. These can be easily confused as pulpal disease; however, the affected teeth are vital and typically are asymptomatic (Figure 12a). Intermediate stage lesions appear partly radiolucent and partly radiopaque with the initiation of hard tissue (bone or cementum) formation in the center of the lesion (Figure 12b). Mature stage lesions appears completely radiopaque (Figure 12c).
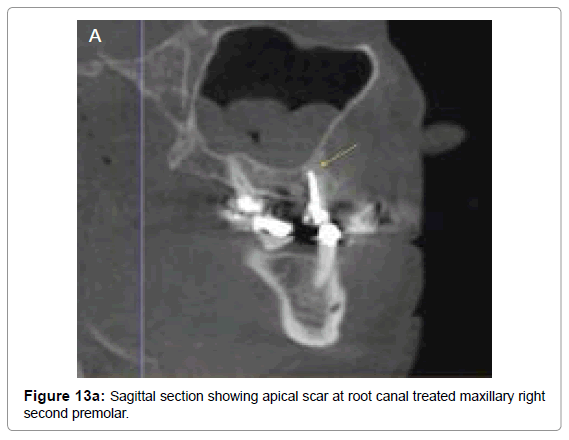
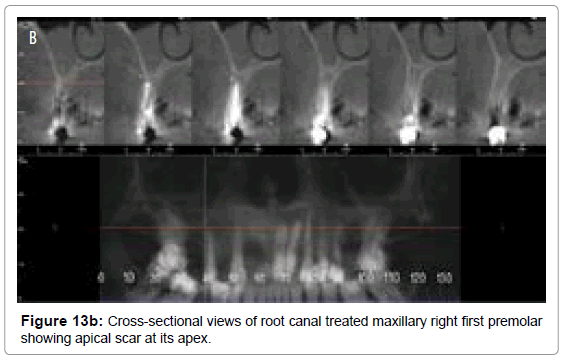
Apical scar results from endodontic treatment of periapical granuloma or abscess, which generally tend to resolve the lesion, but sometimes the granulation tissue produces excessive collagen fibers that results in a dense tissue scar. This remains as a permanent, asymptomatic periapical lesion and appear as a well circumscribed radiolucency on the radiograph (Figure 13a and 13b). Surgical defect/ apical scar also results from failure of osseous tissue formation following surgery at the apex of the tooth. This defect appears as a low density region at apex of the tooth on a radiograph [63].
Resorption is another common periapical condition associated with either a physiologic or a pathologic process resulting in a loss of dentin, cementum, and/or bone [64]. Resorption of the roots of the permanent teeth is a pathological process originating either internally or externally based on the surface of tooth being resorbed.
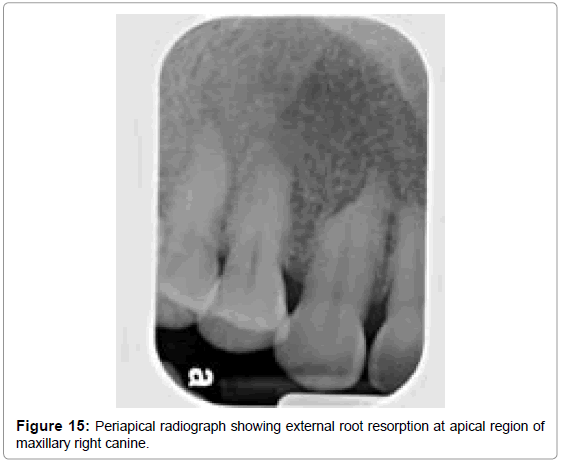
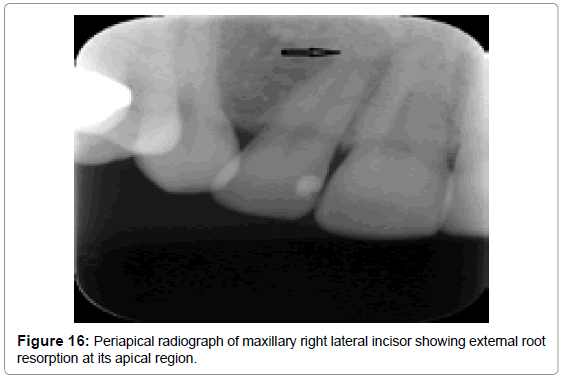
Internal resorption is an inflammatory process initiated within the pulp space with loss of dentin and possible invasion of the cementum [64]. External root resorption occurs when odontoclasts resorb the external surface of the tooth root involving the cementum, dentin and sometime extending to the pulp. Various contributory etiologic factors have been proposed for internal root resorption , but trauma is found to be the most common etiological factor (43%), followed by carious lesions (25%) [65]. Etiology behind the external root resorption is unknown, however, other causes have been attributed such as reimplantation, trauma, and pressure from adjacent unerupted teeth and related pathological conditions such as odontogenic and nonodontogenic tumors.
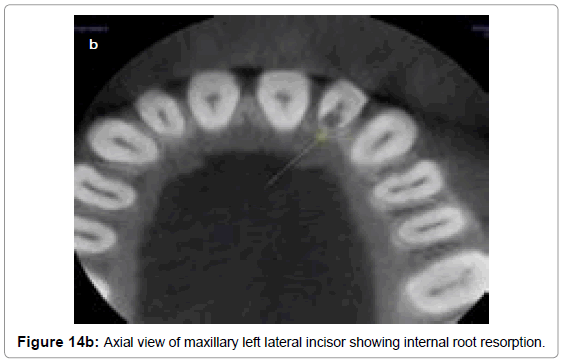
Early lesions of internal resorption are usually asymptomatic and often recognized clinically through routine full mouth radiographs. They appear as localized, oval shape radiolucent enlargement within the pulp chamber or the root canal, as demonstrated in the periapical radiograph (Figure 14a) and the axial view of the same tooth (Figure 14b). In internal resorption, the outline of the root canal is usually distorted and the root canal and the radiolucent resorptive defect appear to be contiguous. External inflammatory root resorption is always accompanied by the resorption of the bone seen as a loss of lamina dura around the apex in addition to that of the root (Figure 15 and 16). External root resorption can also occur along the lateral aspect of the roots due to presence of an unerupted adjacent tooth. When the defect is external, the root canal outline appears normal and can usually be seen ‘running through’ the radiolucent defect.
The early diagnosis of the internal and external root resorptions is difficult based on a conventional radiograph only. CBCT has been found to be successful in evaluating the true nature and severity of resorption lesions [66,67].
There are many other inflammatory, developmental, and benign and malignant cystic and neoplastic lesion that result in periapical osseous defects, those are described elsewhere.
Conclusion
Osseous defects from periodontal and periapical lesions are far more common and are detected routinely as incidental findings. Establishing an accurate diagnosis is always crucial. Intra-oral periapical and bitewing radiographs are superior to extra-oral panoramic radiographs in detecting periodontal and periapical osseous lesions. Three dimensional CBCT scans are considered as a useful complement to these conventional radiographic techniques. Diagnostic benefit and dose detriment tradeoffs are important considerations in choices of radiographic procedures. It is imperative that CBCT be fully justified over conventional techniques for each given case before CBCT is applied for detection of periodontal and periapical lesions.
References
- Baljoon M, Natto S, Abanmy A, Bergström J (2005) Smoking and vertical bone defects in a Saudi Arabian population. Oral Health Prev Dent 3: 173-182.
- Manson JD (1976) Bone morphology and bone loss in periodontal disease. J ClinPeriodontol 3: 14-22.
- Holmlund A, Holm G, Lind L (2006) Severity of periodontal disease and number of remaining teeth are related to the prevalence of myocardial infarction and hypertension in a study based on 4,254 subjects. J Periodontol 77: 1173-1178.
- Kebschull M, Demmer RT, Papapanou PN. (2010) "Gum bug, leave my heart alone!"--epidemiologic and mechanistic evidence linking periodontal infections and atherosclerosis. Journal of dental research 89:879-902.
- Rohlin M, Akerblom A (1992) Individualized periapical radiography determined by clinical and panoramic examination. DentomaxillofacRadiol 21: 135-141.
- Morton TH Jr (1979) Differential diagnosis of periapical radiolucent lesions. Dent Clin North Am 23: 519-541.
- Langen HJ, Fuhrmann R, Diedrich P, Günther RW (1995) Diagnosis of infra-alveolar bony lesions in the dentate alveolar process with high-resolution computed tomography. Experimental results. Invest Radiol 30: 421-426.
- Segura-Egea JJ, Jimenez-Pinzon A, Rios-Santos JV, Velasco-Ortega E, Cisneros-Cabello R, et al. (2008) High prevalence of apical periodontitis amongst smokers in a sample of Spanish adults. International endodontic journal 41:310-316.
- Lopez-Lopez J, Jane-Salas E, Estrugo-Devesa A, Castellanos-Cosano L, Martin-Gonzalez J, et al. (2012) Frequency and distribution of root-filled teeth and apical periodontitis in an adult population of Barcelona, Spain. International dental journal 62:40-46.
- Jiménez-Pinzón A, Segura-Egea JJ, Poyato-Ferrera M, Velasco-Ortega E, Ríos-Santos JV (2004) Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. IntEndod J 37: 167-173.
- Lin LM, Pascon EA, Skribner J, Gängler P, Langeland K (1991) Clinical, radiographic, and histologic study of endodontic treatment failures. Oral Surg Oral Med Oral Pathol 71: 603-611.
- Akesson L, Håkansson J, Rohlin M (1992) Comparison of panoramic and intraoral radiography and pocket probing for the measurement of the marginal bone level. J ClinPeriodontol 19: 326-332.
- Mol A (2004) Imaging methods in periodontology. Periodontol 2000 34: 34-48.
- de FariaVasconcelos K, Evangelista KM, Rodrigues CD, Estrela C, de Sousa TO, et al. (2012) Detection of periodontal bone loss using cone beam CT and intraoral radiography. DentomaxillofacRadiol 41: 64-69.
- van der Stelt PF, Ruttiman UE, Webber RL, Heemstra P (1989) In vitro study into the influence of X-ray beam angulation on the detection of artificial caries defects on bitewing radiographs. Caries Res 23: 334-341.
- Reddy MS (1992) Radiographic methods in the evaluation of periodontal therapy. J Periodontol 63: 1078-1084.
- de Toledo BE, Barroso EM, Martins AT, Zuza EP (2012) Prevalence of Periodontal Bone Loss in Brazilian Adolescents through Interproximal Radiography. Int J Dent 2012: 357056.
- Tugnait A, Carmichael F (2005) Use of radiographs in the diagnosis of periodontal disease. Dent Update 32: 536-538, 541-2.
- van der Stelt PF (2000) Principles of digital imaging. Dent Clin North Am 44: 237-248.
- Sanderink GC (1993) Imaging: new versus traditional technological aids. Int Dent J 43: 335-342.
- MolA (2000) Image processing tools for dental applications. Dent Clin North Am 44: 299-318.
- VandreRH, Webber RL (1995) Future trends in dental radiology. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 80: 471-478.
- Kaeppler G, Vogel A, Axmann-Krcmar D (2000) Intra-oral storage phosphor and conventional radiography in the assessment of alveolar bone structures. DentomaxillofacRadiol 29: 362-367.
- Mol A, Balasundaram A (2008) In vitro cone beam computed tomography imaging of periodontal bone. DentomaxillofacRadiol 37: 319-324.
- Eickholz P, Hausmann E (2000) Accuracy of radiographic assessment of interproximal bone loss in intrabony defects using linear measurements. Eur J Oral Sci 108: 70-73.
- Jeffcoat MK (1994) Current concepts in periodontal disease testing. J Am Dent Assoc 125: 1071-1078.
- Misch KA, Yi ES, Sarment DP (2006) Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol 77: 1261-1266.
- Ramadan AB, Mitchell DF (1962) A roentgenographic study of experimental bone destruction. Oral Surg Oral Med Oral Pathol 15: 934-943.
- Rees TD, Biggs NL, Collings CK (1971) Radiographic interpretation of periodontal osseous lesions. Oral Surg Oral Med Oral Pathol 32: 141-153.
- Hirschmann PN (1987) Radiographic interpretation of chronic periodontitis. Int Dent J 37: 3-9.
- Pope O, Sathorn C1, Parashos P2 (2014) A comparative investigation of cone-beam computed tomography and periapical radiography in the diagnosis of a healthy periapex. J Endod 40: 360-365.
- Tsai P, Torabinejad M, Rice D, Azevedo B (2012) Accuracy of cone-beam computed tomography and periapical radiography in detecting small periapical lesions. J Endod 38: 965-970.
- Chau AC, Fung K (2009) Comparison of radiation dose for implant imaging using conventional spiral tomography, computed tomography, and cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 107: 559-565.
- Ekestubbe A, Thilander A, Gröndahl K, Gröndahl HG (1993) Absorbed doses from computed tomography for dental implant surgery: comparison with conventional tomography. DentomaxillofacRadiol 22: 13-17.
- Lamichane M, Anderson NK, Rigali PH, Seldin EB, Will LA. (2009) Accuracy of reconstructed images from cone-beam computed tomography scans. Am J OrthodDentofacialOrthop136(2):156.e1-6; discussion 156-7.doi: 10.1016/j.ajodo.2009.04.006
- Fuhrmann RA, Bücker A, Diedrich PR (1997) Furcation involvement: comparison of dental radiographs and HR-CT-slices in human specimens. J Periodontal Res 32: 409-418.
- Fuhrmann RA, Wehrbein H, Langen HJ, Diedrich PR (1995) Assessment of the dentate alveolar process with high resolution computed tomography. DentomaxillofacRadiol 24: 50-54.
- Vandenberghe B, Jacobs R, Yang J (2007) Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 104: 395-401.
- Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG (2007) Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 103: 114-119.
- Vizzotto MB, Silveira PF, Arus NA, Montagner F, Gomes BP, da Silveira HE. (2013) CBCT for the assessment of second mesiobuccal (MB2) canals in maxillary molar teeth: effect of voxel size and presence of root filling. International endodontic journal 46:870-876.
- Abuabara A, Baratto-Filho F, AguiarAnele J, Leonardi DP, Sousa-Neto MD. (2013) Efficacy of clinical and radiological methods to identify second mesiobuccal canals in maxillary first molars. ActaodontologicaScandinavica 71:205-209.
- Marmary Y, Kutiner G (1986) A radiographic survey of periapical jawbone lesions. Oral Surg Oral Med Oral Pathol 61: 405-408.
- Horner K (2013) Cone-beam computed tomography: time for an evidence-based approach. Prim Dent J 2: 22-31.
- Theodorakou C, Walker A, Horner K, Pauwels R, Bogaerts R, et al. (2012) Estimation of paediatric organ and effective doses from dental cone beam CT using anthropomorphic phantoms. Br J Radiol 85: 153-160.
- Schauer DA, Linton OW (2009) NCRP Report No. 160, Ionizing Radiation Exposure of the Population of the United States, medical exposure--are we doing less with more, and is there a role for health physicists? Health physics 97:1-5.
- Smith-Bindman R, Miglioretti DL, Larson EB (2008) Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) 27: 1491-1502.
- Ludlow JB, Davies-Ludlow LE, Brooks SL (2003) Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. DentomaxillofacRadiol 32: 229-234.
- Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB (2006) Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. DentomaxillofacRadiol 35: 219-226.
- Ludlow JB, Davies-Ludlow LE, White SC. (2008) Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculation. Journal of the American Dental Association 139:1237-1243.
- Hirsch E, Wolf U, Heinicke F, Silva MA (2008) Dosimetry of the cone beam computed tomography Veraviewepocs 3D compared with the 3D Accuitomo in different fields of view. DentomaxillofacRadiol 37: 268-273.
- Ludlow JB, Ivanovic M (2008) Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 106: 106-114.
- Roberts JA, Drage NA, Davies J, Thomas DW (2009) Effective dose from cone beam CT examinations in dentistry. Br J Radiol 82: 35-40.
- Suomalainen A, Kiljunen T, Kaser Y, Peltola J, Kortesniemi M (2009) Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillo facial radiology 38: 367-378.
- Roberts JA, Drage NA, Davies J, Thomas DW (2009) Effective dose from cone beam CT examinations in dentistry. Br J Radiol 82: 35-40.
- Ludlow JB, Ivanovic M (2008) Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 106: 106-114.
- Pepelassi EA, Tsiklakis K, Diamanti-Kipioti A (2000) Radiographic detection and assessment of the periodontal endosseous defects. J ClinPeriodontol 27: 224-230.
- Newman MG, Takei HH, PKlokkevold PR, Carranza FA (2006) Caranza'sClnical Periodontology. (10 ed). W.B. Saunders Co.: St. Louis.
- Goldman HM, Cohen DW (1958) Theinfrabony pocket: classification and treatment. Journal of periodontology 29:272-276.
- Prichard JF (1967) Theetiology, diagnosis and treatment of the intrabony defect. J Periodontol 38: 455-465.
- Karn KW, Shockett HP, Moffitt WC, Gray JL (1984) Topographic classification of deformities of the alveolar process. J Periodontol 55: 336-340.
- Qiao J, Wang S, Duan J, Zhang Y, Qiu Y, et al. (2014) The accuracy of cone-beam computed tomography in assessing maxillary molar furcation involvement. J ClinPeriodontol 41: 269-274.
- Walter C, Weiger R, Zitzmann NU (2010) Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J ClinPeriodontol 37: 436-441.
- Langlais R, Langland O, Nortje CJ (1995) Diagnostic imaging of the jaws: Lea &Febiger.
- AlbiniRiccioli G (1973) Glossary of endodontic terms drawn up by the endodontic study group. Mondo Odontostomatol 15: 465-468.
- CaliÅŸkan MK (1997) Prognosis of permanent teeth with internal resorption: a clinical review. Endod Dent Traumatol 13: 75-81.
- Cohenca N, Simon JH, Mathur A, Malfaz JM (2007) Clinical indications for digital imaging in dento-alveolar trauma. Part 2: root resorption. Dental traumatology: official publication of International Association for Dental Traumatology 23:105-113.
- Patel S, Dawood A, Wilson R, Horner K, Mannocci F (2009) The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - an in vivo investigation. International endodontic journal 42:831-838.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 35965
- [From(publication date):
November-2014 - Aug 24, 2025] - Breakdown by view type
- HTML page views : 30194
- PDF downloads : 5771