Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
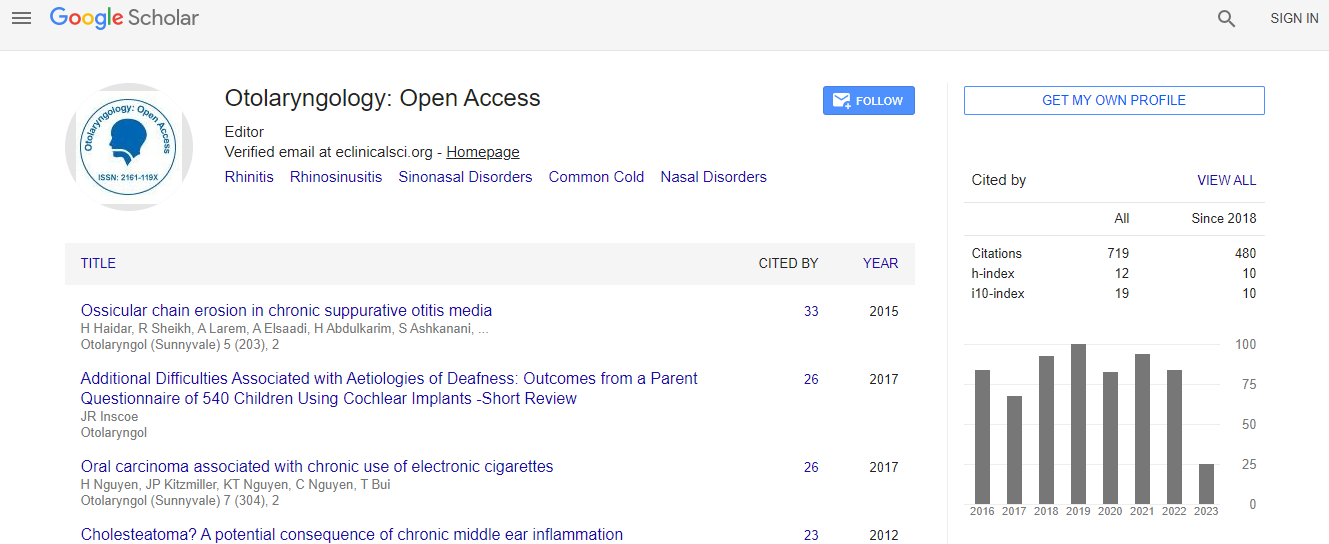
Google Scholar citation report
Citations : 925
Otolaryngology: Open Access received 925 citations as per Google Scholar report
Otolaryngology: Open Access peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Comparison of surgical tracheostomy and percutaneous dilatational tracheostomy in intensive care unit patients
Joint Event on 4th European Otolaryngology-ENT Surgery Conference & 3rd International Conference on Craniofacial Surgery
Inn-chul Nam
The Catholic Universtiy of Korea, Republic of Korea
ScientificTracks Abstracts: Otolaryngol (Sunnyvale)
Abstract
Percutaneous dilatational tracheostomy (PDT) has become an increasingly popular method of establishing an airway for patients in need of chronic ventilator assistance. The aim of this study is to assess and compare two main strategies for doing tracheostomy: traditional open surgical tracheostomy (ST) and PDT. We retrospectively reviewed medical records of 43 patients who underwent tracheostomy between the years 2016 and 2017. All patients were under intensive care unit (ICU) care and referred to the department of otolaryngology for tracheostomy. All tracheostomies were performed at the bedside using either percutaneous dilatational technique or open surgical technique by a single surgeon. In cases of PDT, either blind puncture technique without any guidance or laryngoscopyguided puncture technique was used. Demographic and procedural variables and complications were compared between the two groups. PDT was performed in 29 patients and ST in 14 patients. Of those who underwent PDT, 15 patients received the blind puncture technique and 14 patients laryngoscopy-guided puncture technique. The cricosternal distance was longer and the amount of blood loss and duration of the procedure was lesser in the PDT group. In the PDT group, there was no difference in blood loss nor in the duration of the procedure according to the puncture technique, whereas critical complications occurred more frequently when the blind technique was used. Subjective difficulty of the procedure is predictive of complications. The study show that PDT is a useful and safe procedure for ICU patients. Also, guidance on using the flexible laryngoscopy during PDT can prevent severe complications.Biography
Dr. Inn-chul Nam has completed his MD from The Catholic University of Korea and acquired PhD from the same institute. He is the assistant professor of The Catholic University of Korea, College of Medicine. He has been serving as the head surgeon of the division of Head and Neck Surgery, Department of ORL-HNS of Incheon St. Mary`s Hospital.
E-mail: entnam@catholic.ac.kr

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi