Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
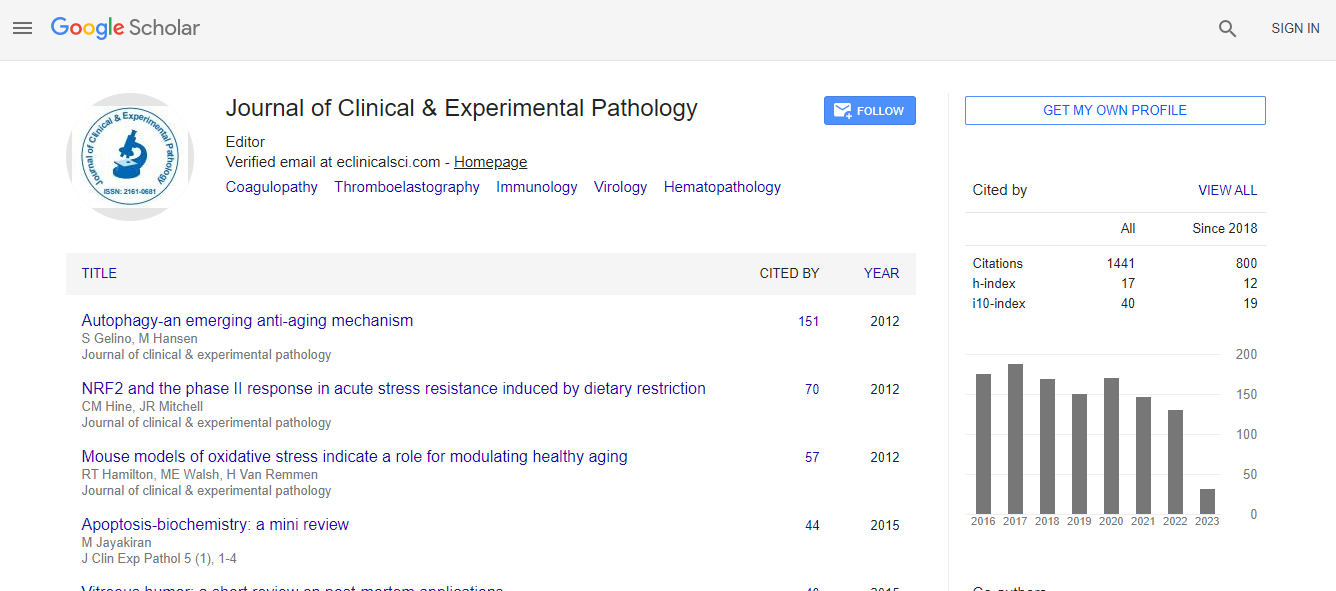
Google Scholar citation report
Citations : 2975
Journal of Clinical & Experimental Pathology received 2975 citations as per Google Scholar report
Journal of Clinical & Experimental Pathology peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Cosmos IF
- Ulrich's Periodicals Directory
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
- world cat
- journal seek genamics
- j-gate
- esji (eurasian scientific journal index)
Useful Links
Recommended Journals
Related Subjects
Share This Page
Diagnostic challenges in lung neuroendocrine tumors
13th International conference on Pathology and Molecular Diagnosis
Mark Podberezin
University of Saskatchewan, Canada
ScientificTracks Abstracts: J Clin Exp Pathol
Abstract
Neuroendocrine tumors (NET) of the lung constitute approximately 15% of all lung tumors, with small cell lung cancer (SCLC) accounting for 15% of invasive cancers. Many of those tumors have radiological and clinical presentation which is different from other pulmonary malignancies. In most cases, diagnosis could be established by core needle biopsy and, not uncommonly, SCLC is detected by endoscopic bronchial ultrasound fine needle aspiration (EBUS-FNA). Spectrum of lung NETs includes typical carcinoid (TC), atypical carcinoid (AC), SCLC and large cell neuroendocrine carcinoma (LCNEC). Morphological criteria, separating low grade from high grade NETs, include cellular atypia, mitotic rate, and presence or absence of necrosis. The question, which has been yet unanswered and which is addressed in the presentation, is whether the above NETs represent continuum from low to high grade tumors or they are biologically different. One of the major diagnostic challenges in pulmonary NETs is their grading on core needle biopsies (CNB). It has been shown that morphological features of NET, when diagnosed by CNB, could be significantly different from the ones on same tumor upon subsequent surgical resection. This could be partially due to marked crush and processing artifact which markedly affect evaluation of mitotic rate. Measurement of proliferative rate by immunohistochemical stain for Ki67 has been approved for grading of NET in the gastrointestinal tract, but is not universally accepted in pulmonary NET. However, it can be very helpful in evaluation of CNB with marked cautery and crush artifact. In addition, CNBs may not be representative of the entire lesion and can lead to diagnostic pitfalls which will be discussed in the presentation.Biography
Mark Podberezin has completed his Medical School Degree (MD) and subsequent Clinical Hematology/Oncology training and PhD in Russia. Later, he did his Residency in Anatomic and Clinical Pathology at University of Illinois at Chicago and Hematopathology Fellowship at Texas Methodist Hospital in Houston. He is an Anatomic Pathologist (with special interest in Lung Pathology) and Hematopathologist at Royal University Hospital, University of Saskatchewan, Canada. He published 14 papers and presented at national, as well as international meetings.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi