Our Group organises 3000+ Global Conferenceseries Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
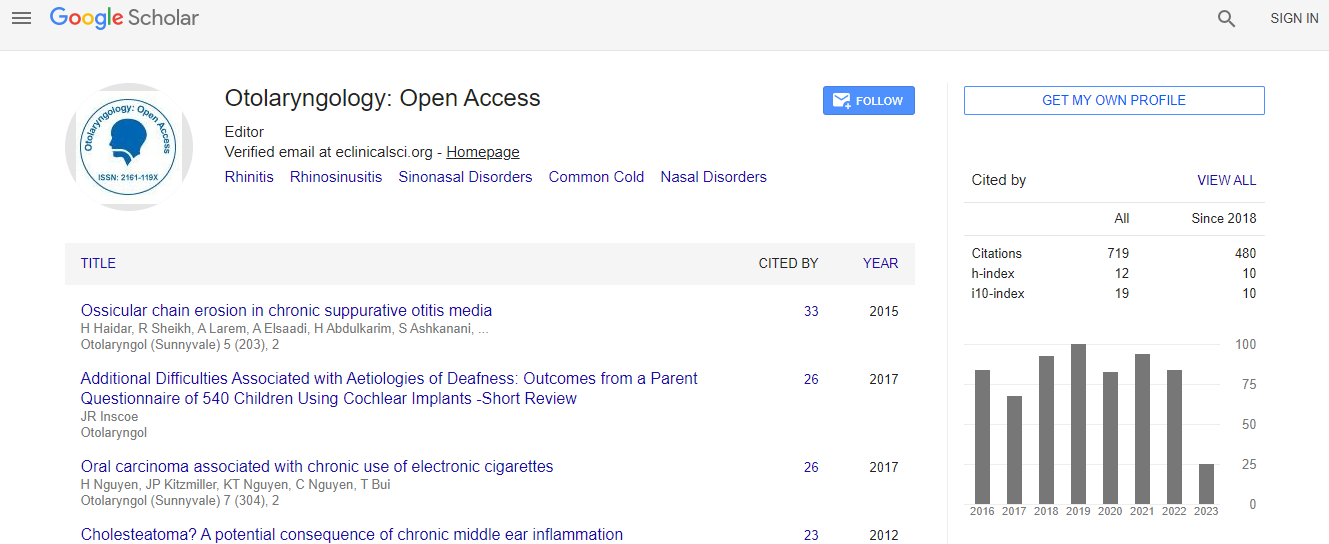
Google Scholar citation report
Citations : 925
Otolaryngology: Open Access received 925 citations as per Google Scholar report
Otolaryngology: Open Access peer review process verified at publons
Indexed In
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Late onset salivary fistula: Rare complication of neurosurgical procedure
3rd International Conference and Exhibition on Rhinology & Otology
Isabelle Nibelle
Al Ain Hospital, UAE
Posters & Accepted Abstracts: Otolaryngology
Abstract
Introduction: Salivary fistula is a common complication in oncology neck surgery. However, this is an unusual outcome after neurosurgical procedure with cervical approach. We report a case of late onset salivary fistula occurring after cervical spinal fixation following a fracture C5C6. We analyze the risk factors. We discuss the diagnostic and therapeutic choices. Finally, we insist on preventing this complication. Material & Method: A 21 year old patient was admitted with quadriplegia after a neck trauma. The injury was a fracture dislocation-C6 / C7 with narrowing of the posterior wall. A neurosurgical surgery is performed in emergency by right anterior cervical approach: decompression of the posterior wall, vertebral fixation with screws C5 to C7, bone graft, laminectomy at C6 and partial facetectomy.A tracheostomy is performed in the same surgical time. Postoperative feeding is provided by nasogastric tube. The patient developed day 43 postoperative a cervical collection, which is simply drained by general surgeons. Collection reccures, associated with clear right paratracheal discharge. Clinical examination is in favor of a salivary fistula. A hydrosoluble hypo pharyngeal transit confirms the continuity between the pharynx and the cervical skin. Direct laryngoscopy confirms the fistula with hypopharyngeal mucosa breach, at the retro-cricoid area with exposure of cervical fixation material. Esophagus is intact. Percutaneous gastrostomy is performed at the same time. Local care with compressive dressing cannot dry the fistula. Surgical closure is performed at day 79 from the initial surgery: The exposure of the previous ostheosyntesis materiel reveals that two screws are loose. The anterior fixation material is removed. Visualization of the salivary fistula at the level of the retro-cricoid area; Hypo pharyngeal mucosa is closed with intermittent stiches with Vicryl 3.0. Coverage performs with local sternocleidomastoid muscle flap with upper and lower attachment. No postoperative event; no recurrence of the fistula. Discussion: Late onset salivary fistula in neck surgery is an unusual complication after neurosurgical approach. In this case, several risk factors have been identified: The presence of tracheotomy, as a factor of compression, nutrition by nasogastric tube as a factor of compression, denutrition as a general condition and the presence of mobile screws, as a friction factor which resulted in the damage of the hypo pharyngeal mucosa. The diagnosis of a salivary fistula is based on: Clinical arguments, biological level of amylase on the discharge, hypo pharyngeal transit with hydrololules: communication between hypopharynx and skin and direct laryngoscopy: visualization of the fistula. Treatment is based on: Local care: twice a day dressing with washing, swallowing diluted betadine and compression bandages, Surgery if failure of the dressing to repair mucosa and coverage flap. Local: sternocleidomastoid muscle or platysmamuscle flap. Regional: pectoralis major and latissimus dorsi flap and free: antebrachial flap Conclusion: Late onset salivary fistulas are rare in non-neoplastic pathologies but may complicate neurosurgical cervical spine surgery with cervical approach. Diagnostic has to be done in front of cervical collection associated with chronic cervical discharge. The treatment begins with twice-daily dressing and, in case of failure, surgery. Prevention is based on reducing risk factors: avoid prolonged nasogastric nutrition, promote high-calorie, high protein nutrition in vulnerable subjects, ensure adequate fixation.Biography
Isabelle Nibelle has completed her PhD in France at the University of Strasbourg and Post-doctoral studies in Paris. She is Head of the ENT department in Al Ain Hospital, UAE and is teaching as Adjunct Assistant Professor at the UEA College of Medicine and Health Sciences.
Email: isabelle@seha.ae

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi